HPA Axis Dysregulation and Neuroendocrine Interactions: From Molecular Mechanisms to Therapeutic Interventions in Stress Pathophysiology
This comprehensive review synthesizes current research on the hypothalamic-pituitary-adrenal (HPA) axis as the central regulator of the stress response and its complex interactions with other neuroendocrine systems.
HPA Axis Dysregulation and Neuroendocrine Interactions: From Molecular Mechanisms to Therapeutic Interventions in Stress Pathophysiology
Abstract
This comprehensive review synthesizes current research on the hypothalamic-pituitary-adrenal (HPA) axis as the central regulator of the stress response and its complex interactions with other neuroendocrine systems. Targeting researchers, scientists, and drug development professionals, the article explores foundational HPA axis physiology, developmental programming, and cross-system communication with reproductive, immune, and gut-brain pathways. It examines methodological approaches for investigating HPA axis function, analyzes mechanisms of stress-induced dysregulation across physiological systems, and evaluates comparative interactions with parallel neuroendocrine axes. The review highlights emerging therapeutic targets and translational applications for disorders linked to HPA axis dysfunction, including autoimmune, metabolic, psychiatric, and reproductive conditions.
Core Architecture and System Integration of the Neuroendocrine Stress Response
The hypothalamic-pituitary-adrenal (HPA) axis serves as the body's primary neuroendocrine system for maintaining homeostasis in the face of real or perceived challenges. This sophisticated axis coordinates adaptive responses to physical, psychological, and immunological stressors through a cascade of hormonal signals culminating in glucocorticoid secretion. Within the broader context of stress research, understanding the HPA axis's intricate architecture and regulatory mechanisms is paramount for elucidating the pathophysiological basis of numerous stress-related disorders and developing novel therapeutic interventions. The HPA axis represents a critical interface between the nervous and endocrine systems, translating neural signals into hormonal outputs that regulate diverse physiological processes including metabolism, immune function, cardiovascular tone, and behavior [1] [2]. This technical guide provides a comprehensive examination of HPA axis anatomy, physiology, and research methodologies, with particular emphasis on the pivotal role of the paraventricular nucleus (PVN) in initiating and modulating the stress response.
Anatomical Architecture of the HPA Axis
The Paraventricular Nucleus (PVN): Central Command
The hypothalamic paraventricular nucleus (PVN) serves as the prime regulator of the HPA axis, housing the neurosecretory neurons that initiate the stress response cascade. The PVN contains three functionally distinct neuronal populations:
- Parvocellular neurosecretory neurons: These CRH-producing neurons project to the median eminence and constitute the primary drivers of the HPA axis [3]
- Magnocellular neurosecretory neurons: These primarily produce oxytocin and vasopressin and project to the posterior pituitary [3]
- Long-projecting neurons: These regulate autonomic function through projections to the brainstem and spinal cord [3]
The development and differentiation of PVN neurons are governed by specific transcription factors. Brn-2 is essential for terminal differentiation of both parvocellular and magnocellular neurons, while Otp and Sim1 regulate the maturation of neurosecretory neurons expressing CRH, AVP, TRH, and oxytocin [3]. Sim1 knockout mice demonstrate severe reductions in CRH, AVP, and OT neurons and rarely survive to adulthood, highlighting this factor's critical role in PVN development [3].
Pituitary Gland: The Relay Center
The pituitary gland consists of two embryologically and functionally distinct components:
- Adenohypophysis (anterior pituitary): Derived from Rathke's pouch, this structure contains specialized hormone-producing cells including corticotropes that synthesize and secrete adrenocorticotropic hormone (ACTH) [3]
- Neurohypophysis (posterior pituitary): Originating from the ventral diencephalon, this region stores and releases oxytocin and vasopressin produced by PVN and supraoptic nucleus (SON) magnocellular neurons [3]
Corticotropes in the anterior pituitary express receptors for CRH and AVP, allowing them to respond to hypothalamic signals by releasing ACTH into the systemic circulation.
Adrenal Cortex: Glucocorticoid Production
The adrenal cortex represents the final endocrine component of the HPA axis. Upon stimulation by ACTH, the zona fasciculata of the adrenal cortex synthesizes and secretes glucocorticoids (cortisol in humans, corticosterone in rodents). ACTH binds to melanocortin 2 receptors (MC2R), activating adenylate cyclase and increasing intracellular cAMP levels [1]. This signaling cascade enhances cholesterol transport into mitochondria via the steroidogenic acute regulatory (StAR) protein, which represents the rate-limiting step in glucocorticoid synthesis [1].
Table 1: Major Components of the HPA Axis
| Anatomical Structure | Key Cell Types | Secreted Factors | Primary Functions |
|---|---|---|---|
| Paraventricular Nucleus (PVN) | Parvocellular neurosecretory neurons | CRH, AVP | Initiate HPA axis activation; regulate ACTH secretion |
| Anterior Pituitary | Corticotropes | ACTH | Stimulate glucocorticoid production in adrenal cortex |
| Adrenal Cortex | Zona fasciculata cells | Glucocorticoids (cortisol/corticosterone) | Mediate widespread metabolic and immune effects |
Physiological Mechanisms and Signaling Pathways
The Neuroendocrine Cascade
HPA axis activation follows a sequential hormonal cascade initiated at the level of the PVN:
- CRH and AVP Release: Parvocellular neurons secrete corticotropin-releasing hormone (CRH) and arginine vasopressin (AVP) into the hypophysial portal system at the median eminence [4]
- ACTH Secretion: CRH and AVP travel to the anterior pituitary where they act synergistically on corticotropes. CRH binds to CRH-R1 receptors, activating adenylate cyclase and increasing cAMP production, while AVP binds to V1b receptors, activating protein kinase C [1] [4]
- Glucocorticoid Production: ACTH stimulates the adrenal cortex to synthesize and secrete glucocorticoids, which exert widespread effects on energy metabolism, immune function, and neural activity [1]
CRH functions as the principal ACTH secretagogue, as evidenced by studies demonstrating that CRH knockout mice show severely impaired basal and stress-induced ACTH release [1]. AVP alone has minimal effect on ACTH secretion but potently synergizes with CRH to amplify corticotrope response [4].
Neurotransmitter Regulation of PVN Activity
The PVN receives extensive innervation from multiple brain regions that convey information about various stressors. These inputs release neurotransmitters that precisely regulate the activity of CRH neurons:
- Excitatory inputs: Glutamate, norepinephrine, and serotonin typically increase CRH neuronal excitability [5]
- Inhibitory inputs: GABA represents the primary inhibitory neurotransmitter regulating PVN activity [5]
Additional modulators include dopamine, acetylcholine, and various neuropeptides that fine-tune the stress response [5]. This complex innervation allows for integration of diverse sensory and interoceptive signals that collectively determine HPA axis output.
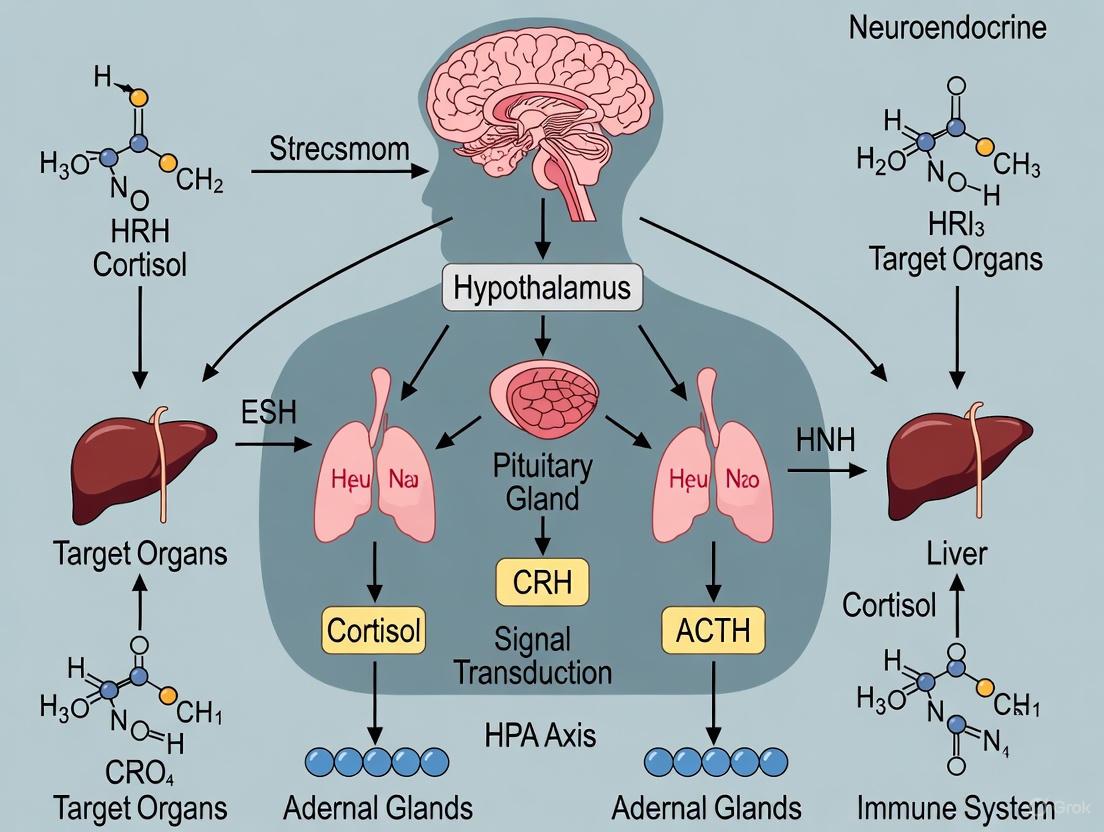
The following diagram illustrates the core signaling pathway of the HPA axis and its regulatory inputs:
Figure 1: Core HPA Axis Signaling Pathway. This diagram illustrates the sequential activation of the HPA axis from hypothalamic PVN to systemic cortisol release, including negative feedback mechanisms that regulate the stress response.
Circadian Regulation and Stress Response Patterns
The HPA axis demonstrates a pronounced circadian rhythm independent of stress exposure. Under basal conditions, glucocorticoid secretion follows a diurnal pattern with peak levels occurring during the active phase (morning in humans, evening in rodents) [2]. This circadian variation is regulated by the suprachiasmatic nucleus (SCN), which provides synaptic input to the PVN and helps synchronize HPA activity with the light-dark cycle [2].
Stress-induced HPA activation follows distinct patterns depending on stressor characteristics:
- Reactive responses: Direct homeostatic challenges (e.g., physical threat, immune activation) typically engage brainstem noradrenergic pathways that directly stimulate PVN neurons [1]
- Anticipatory responses: Psychological stressors activate oligosynaptic pathways originating in limbic structures (e.g., hippocampus, prefrontal cortex, amygdala) that modulate PVN activity largely through disinhibition mechanisms [1]
The magnitude and duration of HPA activation vary according to stressor intensity, controllability, predictability, and novelty [2].
Regulatory Mechanisms and Feedback Loops
Glucocorticoid Receptor Signaling and Negative Feedback
Glucocorticoids exert potent negative feedback on the HPA axis at multiple levels to limit the duration and magnitude of stress responses. This feedback occurs through three temporal domains:
- Fast feedback: Occurs within minutes, mediated by non-genomic glucocorticoid actions likely involving membrane-associated receptors [4]
- Intermediate feedback: Involves glucocorticoid modulation of post-translational processing and release of pre-formed peptides [2]
- Slow feedback: Occurs over hours to days and involves genomic actions mediated by cytosolic glucocorticoid receptors (GR) that alter gene transcription [1]
At the PVN, fast feedback inhibition of CRH neurons is mediated by glucocorticoid-dependent mobilization of endocannabinoids, which act as retrograde messengers to suppress presynaptic glutamate release via CB1 receptors [4]. Additional feedback sites include the pituitary gland, where glucocorticoids inhibit ACTH synthesis and secretion, and higher brain centers such as the hippocampus and prefrontal cortex, which provide inhibitory input to the PVN [1].
Heterosynaptic Modulation in the PVN
The PVN exhibits sophisticated heterosynaptic modulation wherein one neurotransmitter system alters the efficacy of another in regulating CRH neuronal activity. This occurs through both presynaptic and postsynaptic mechanisms:
- Presynaptic heterosynaptic modulation: Involves alteration of neurotransmitter release from terminals, often through actions on presynaptic receptors [5]
- Postsynaptic heterosynaptic modulation: Occurs when a neurotransmitter modifies the postsynaptic response to another neurotransmitter, frequently through signal transduction pathways that regulate receptor sensitivity or membrane excitability [5]
For example, norepinephrine can enhance GABAergic transmission onto CRH neurons via α1-adrenoceptors, while serotonin inhibits GABA release through 5-HT1A receptors [5]. This heterosynaptic integration allows for sophisticated computation of diverse stress-related signals within the PVN microcircuitry.
Experimental Models and Methodologies
Assessment of HPA Axis Function
Research investigating HPA axis physiology employs diverse methodological approaches across multiple levels of analysis:
Table 2: Experimental Methods for HPA Axis Investigation
| Analysis Level | Technical Approaches | Measured Parameters |
|---|---|---|
| Molecular | RT-PCR, in situ hybridization, Western blot, ELISA | CRH/AVP mRNA and protein, receptor expression, glucocorticoid levels |
| Neuroanatomical | Immunohistochemistry, tract tracing, electron microscopy | Neuronal activation (c-Fos), connectivity, synaptic ultrastructure |
| Physiological | Radioimmunoassay, HPLC, microdialysis | Hormone levels, neurotransmitter release, heart rate, blood pressure |
| Functional | Pharmacological challenges, electrophysiology, optogenetics | Neuronal excitability, hormone responses to stimuli, feedback sensitivity |
Chronic Stress Paradigms
Studies investigating maladaptive HPA axis regulation frequently employ chronic stress models including:
- Chronic variable stress: Exposure to unpredictable stressors over days to weeks [4]
- Chronic social defeat: Repeated exposure to aggressive conspecifics [1]
- Restraint/immobilization stress: Repeated physical confinement [6]
These paradigms produce neuroplastic adaptations including increased CRH and AVP expression in the PVN, enhanced excitatory innervation of CRH neurons, reduced GABAergic inhibition, and diminished glucocorticoid feedback efficacy [4]. The following diagram illustrates a typical experimental workflow for investigating HPA axis function in rodent models:
Figure 2: Experimental Workflow for HPA Axis Research. This diagram outlines a comprehensive approach to investigating HPA axis function in preclinical models, integrating molecular and physiological analyses.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for HPA Axis Investigation
| Reagent/Chemical | Specific Example | Research Application |
|---|---|---|
| CRH-R1 Antagonist | NBI-27914 | Selective blockade of CRH type 1 receptors to investigate CRH signaling [6] |
| Adrenergic Receptor Ligands | Prazosin (α1-antagonist), propranolol (β-antagonist) | Dissection of catecholaminergic influences on PVN neuronal activity [5] |
| GABA Receptor Modulators | Bicuculline (GABA-A antagonist), baclofen (GABA-B agonist) | Investigation of inhibitory control of CRH neurons [6] [5] |
| Glucocorticoid Receptor Agonists/Antagonists | RU28362 (GR agonist), RU486 (GR antagonist) | Assessment of glucocorticoid feedback mechanisms [1] |
| Corticosterone/Cortisol Assays | ELISA, RIA kits | Quantification of circulating glucocorticoid levels [6] |
| Neuroanatomical Tracers | Fluorogold, cholera toxin B | Mapping of afferent and efferent connections of PVN neurons [4] |
Pathophysiological Implications and Research Applications
Dysregulation of the HPA axis represents a central feature in numerous pathological conditions:
- Neuropsychiatric disorders: Depression, PTSD, and anxiety disorders are associated with altered HPA axis activity, including CRH hypersecretion, glucocorticoid resistance, and impaired negative feedback [7] [8]
- Autoimmune diseases: Chronic stress-induced HPA dysfunction can promote inflammatory responses and contribute to conditions such as rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis [7]
- Metabolic disorders: Prolonged glucocorticoid excess promotes hepatic glycogenolysis, lipolysis, and insulin resistance, contributing to metabolic syndrome [7]
- Neurodegenerative disorders: Chronic glucocorticoid exposure can damage hippocampal neurons and impair cognitive function [8]
Recent research has identified pituitary adenylate cyclase-activating polypeptide (PACAP) as an important regulator of stress responses, with specific gene polymorphisms in the ADCYAP1 gene associated with PTSD vulnerability, particularly in women [9] [10]. This discovery highlights the potential for targeting novel neuropeptide systems in the development of future stress-related therapeutics.
The intricate organization and regulation of the HPA axis underscores its fundamental role in maintaining physiological homeostasis amid changing environmental demands. Continued investigation of PVN circuitry, neuropeptide signaling, and glucocorticoid receptor function will undoubtedly yield critical insights for developing targeted interventions for the myriad disorders associated with HPA axis dysregulation.
The Developmental Origins of Health and Disease (DOHaD) hypothesis posits that environmental exposures during sensitive developmental windows program physiological systems, influencing lifelong disease susceptibility [11]. At its core, this hypothesis suggests that early-life adaptations enhance short-term survival but may increase the risk of chronic diseases over decades [11]. The hypothalamic-pituitary-adrenal (HPA) axis, a central stress response and homeostatic system, is one of the key fetal systems most sensitive to these programming effects [11] [12]. Prenatal programming of the fetal HPA axis is proposed as a primary mechanism linking early experiences to later disease risk [12]. During gestation, the developing fetal brain exhibits remarkable plasticity, making it highly susceptible to maternal, placental, and other intrauterine signals [12]. If these signals indicate conditions of deprivation or stress, the fetus adjusts its developmental trajectory, potentially at a cost to long-term health, especially if a mismatch occurs between the predicted and actual postnatal environment [12].
Table 1: Key Concepts in Developmental Programming of the HPA Axis
| Concept | Description | Implication |
|---|---|---|
| Developmental Plasticity | Ability of a single genotype to produce different phenotypes in response to environmental conditions [11]. | Allows for adaptive calibration of HPA axis set-points to the anticipated environment. |
| Critical Window | A specific developmental period during which the system is most susceptible to programming influences [12]. | Explains the time-sensitive nature of HPA axis programming by early-life exposures. |
| Fetal Programming | The process by which an environmental stimulus during a sensitive developmental period has a lasting impact on the structure and function of organ systems [12]. | Provides a mechanistic link between the prenatal environment and adult health. |
| Mismatch Hypothesis | The concept that disease risk arises when the prenatally predicted environment differs from the actual postnatal environment [12]. | Explains why early adaptive changes can become maladaptive later in life. |
HPA Axis Physiology and Development
The Functional HPA Axis
The mature HPA axis is a neuroendocrine system that regulates the body's physiological and psychological adaptation to stress. Its activation involves a coordinated cascade: in response to a stressor, the paraventricular nucleus (PVN) of the hypothalamus secretes corticotropin-releasing hormone (CRH) and arginine vasopressin (AVP) into the hypophyseal portal system [11] [13] [12]. These hormones stimulate the anterior pituitary gland to release adrenocorticotropic hormone (ACTH), which in turn prompts the adrenal cortex to secrete the glucocorticoid cortisol into the systemic circulation [11] [13] [12]. Circulating cortisol exerts widespread effects, including on metabolism, immune function, and cognition, and primarily regulates its own secretion through a negative feedback loop by binding to glucocorticoid receptors (GR) and mineralocorticoid receptors (MR) in the hippocampus, hypothalamus, and pituitary to inhibit further CRH and ACTH release [13] [12].
HPA Axis Signaling Pathway
Developmental Timeline of the HPA Axis
The construction of the HPA axis is an intricate process that begins early in fetal life. The hypothalamus derives from the anteroventral neuroectoderm, with key transcription factors like Brn-2, Otp, and Sim1 regulating the differentiation of CRH-producing neurons in the PVN [3]. The pituitary gland develops from a dual origin—the oral ectoderm forms Rathke's pouch (anterior pituitary), while the neural ectoderm gives rise to the posterior pituitary [3]. The fetal adrenal cortex is distinct, featuring a large fetal zone that produces precursor steroids; this zone involutes after birth, and the adult adrenal architecture with its three distinct zones—zona glomerulosa, zona fasciculata, and zona reticularis—matures postnatally, with the zona reticularis becoming fully formed around adrenarche [14]. The fetal HPA axis does not develop in isolation but is part of an integrated maternal-placental-fetal (MPF) unit [12]. The human placenta produces CRH identical to hypothalamic CRH, and unlike the negative feedback in the mature brain, maternal cortisol stimulates placental CRH production, creating a unique positive feedback loop that drives a substantial increase in maternal and fetal glucocorticoid levels over gestation [12].
Table 2: Critical Windows in Human HPA Axis Development
| Developmental Stage | Key Developmental Events | Vulnerability to Programming |
|---|---|---|
| First Trimester | Hypothalamic primordium differentiation; pituitary gland formation; placental CRH production begins [3] [12]. | Foundation for entire stress axis is laid; exposure to synthetic glucocorticoids or extreme maternal stress can disrupt initial organization. |
| Second Trimester | Prolific neurogenesis and neuronal migration; establishment of basic HPA circuitry [12]. | System is highly plastic; maternal nutrition and stress can influence neuronal connectivity and receptor density. |
| Third Trimester | Exponential rise in placental CRH; maturation of negative feedback mechanisms; fetal zone of adrenal is active [12]. | High glucocorticoid exposure can program the set-point for stress sensitivity and feedback efficiency. |
| Early Postnatal Period | Involution of fetal adrenal zone; establishment of adult adrenal zonation; refinement of feedback loops [14]. | The postnatal environment can reinforce or counteract prenatal programming; caregiver interaction is critical. |
Mechanisms of Developmental Programming
Pathways of Prenatal Influence
The fetal HPA axis can be programmed by several maternal and placental factors, with glucocorticoids acting as a final common pathway. The primary mechanisms include:
- Maternal Glucocorticoid Exposure: Maternal stress, whether physiological or psychological, can lead to elevated maternal cortisol. This cortisol can cross the placenta and access the fetal circulation, potentially altering the development of fetal brain structures involved in HPA regulation, such as the hippocampus, amygdala, and PVN [11] [12]. The enzyme 11β-hydroxysteroid dehydrogenase type 2 (11β-HSD2), which acts as a placental barrier by inactivating cortisol, can be downregulated by maternal stress or malnutrition, further increasing fetal exposure [11].
- Placental CRH Drive: The placenta, by producing ever-increasing amounts of CRH throughout gestation, is a major driver of the maternal and fetal steroidogenic environment [12]. Elevated placental CRH has been linked to preterm birth and may precondition the fetal HPA axis to be more reactive after birth.
- Epigenetic Modifications: Early-life exposures can induce stable changes in gene expression without altering the DNA sequence. For instance, maternal diet (e.g., choline intake) and stress have been shown to alter the DNA methylation status of genes encoding the glucocorticoid receptor and 11β-HSD2, thereby changing their expression levels and influencing HPA axis function long-term [11].
Key Programming Exposures and Experimental Evidence
Research has identified specific maternal exposures that consistently lead to HPA axis programming in offspring.
- Maternal Nutrition: Animal models consistently show that maternal protein or caloric restriction elevates basal HPA tone and the dynamic stress response in offspring, often via changes in central glucocorticoid receptor expression [11]. Human studies, such as those on the Dutch Hunger Winter, have shown that prenatal undernutrition is associated with altered HPA axis reactivity in offspring six decades later [11].
- Mental Health and Chronic Stress: Maternal anxiety and depression during pregnancy are associated with higher placental CRH levels and have been linked to altered cortisol responses in infants and children [12]. Chronic stress can lead to a dysregulated HPA axis characterized by impaired negative feedback.
- Maternal Obesity and Metabolic State: Maternal obesity and high maternal lipid levels have been associated with increased cortisol reactivity in children, suggesting that the metabolic environment can also program the stress axis [11].
Experimental Methodologies for Investigating HPA Axis Programming
Human Study Designs and Protocols
Prospective longitudinal cohort studies are the gold standard for investigating HPA axis programming in humans. The general workflow involves recruiting pregnant women, extensively characterizing their prenatal environment, and then following their offspring from birth into adulthood to assess HPA axis function at multiple time points.
HPA Programming Research Workflow
Detailed Protocol for a Longitudinal Birth Cohort Study:
Prenatal Assessment (During each trimester):
- Maternal Questionnaires: Administer validated instruments to assess psychological stress (e.g., Perceived Stress Scale), anxiety (e.g., State-Trait Anxiety Inventory), diet (e.g., food frequency questionnaires), and lifestyle factors.
- Maternal Biological Sampling: Collect maternal saliva, blood, and/or urine.
- Salivary Cortisol: Participants collect saliva at home at specified times (e.g., upon waking, 30 minutes post-waking, before lunch, before bed) over 1-2 days to assess diurnal cortisol rhythm [12].
- Plasma/Serum: Analyze for placental CRH, ACTH, cortisol, and inflammatory markers. Samples are typically processed within 2 hours and stored at -80°C.
- Urine: Assess for catecholamines as a measure of sympathetic activity.
Neonatal Assessment (At Birth):
- Placental Collection: Immediately after delivery, collect placental tissue biopsies from standardized locations (e.g., central cotyledon, free membranes). Flash-freeze a portion in liquid nitrogen for RNA/protein analysis (e.g., CRH gene expression, 11β-HSD2 activity) and preserve another portion in formalin for histology.
- Cord Blood Collection: Collect umbilical cord blood from the umbilical vein. Process to obtain plasma/serum and analyze for cortisol, ACTH, and CRH levels.
Postnatal HPA Axis Assessment in Offspring (e.g., at 6, 12, 24 months):
- Diurnal Cortisol: Parents collect child's saliva at specified times (e.g., waking, pre-nap, post-nap, bedtime) on 1-2 days.
- Stress Reactivity Protocols: Conduct mild, standardized laboratory stressor tests suitable for the age group.
- Infants: The "Still-Face Paradigm," where the parent interacts normally, then maintains a neutral still face for 2 minutes, before resuming normal interaction. Saliva is collected pre-, immediately post-, and 20-minutes post-stressor to measure cortisol response [12].
- Older Children/Adults: The Trier Social Stress Test for Children (TSST-C), which involves a public speaking and mental arithmetic task in front of an audience. Saliva or blood is collected at baseline, immediately post-task, and at multiple recovery timepoints (e.g., +10, +20, +30, +45 mins) to model the cortisol response curve, including peak response and recovery slope [11] [12].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Research Reagents for HPA Axis Programming Studies
| Reagent/Material | Function/Application | Example Use in Protocol |
|---|---|---|
| Corticotropin-Releasing Hormone (CRH), Antibodies | To detect and quantify CRH protein or mRNA expression in placental or brain tissue. | Immunohistochemistry on placental sections; ELISA for plasma CRH; qPCR for CRH mRNA. |
| Cortisol ELISA/EIA Kits | To measure cortisol concentration in biological fluids (saliva, serum, plasma, urine). | Quantifying diurnal cortisol profiles and stress-induced cortisol responses in maternal and offspring samples. |
| ACTH Chemiluminescence Immunoassay | To measure ACTH levels in plasma, requiring careful sample handling due to peptide instability. | Assessing pituitary response in the HPA axis cascade, often in conjunction with cortisol measures. |
| DNA Methylation Analysis Kits (e.g., Bisulfite Conversion) | To prepare DNA for analysis of epigenetic modifications, such as methylation of the glucocorticoid receptor gene (NR3C1) promoter. | Investigating epigenetic mechanisms by which prenatal stress programs the offspring HPA axis. |
| RNA Extraction Kits & qPCR Reagents | To isolate and quantify gene expression levels of HPA axis components (e.g., GR, MR, CRH, POMC). | Analyzing gene expression in post-mortem brain tissue (animal models) or peripheral blood cells. |
| 11β-HSD2 Activity Assay | To measure the enzymatic activity that converts active cortisol to inactive cortisone. | Determining the placental barrier capacity to glucocorticoids using placental tissue homogenates. |
| Validated Psychometric Scales | Standardized questionnaires to quantify psychological constructs. | Assessing maternal prenatal stress, anxiety, and depression levels (e.g., PSS, STAI). |
Lifelong Consequences of HPA Axis Programming
The maladaptive programming of the HPA axis is a significant risk factor for a spectrum of disorders across the lifespan. The consequences are not limited to mental health but encompass physical health domains as well.
- Neuropsychiatric Disorders: HPA axis hyperactivity and impaired negative feedback are well-documented in Major Depressive Disorder (MDD) [15]. Programmed hypercortisolemia can lead to neuronal damage and atrophy in brain regions rich in GR receptors, such as the hippocampus and prefrontal cortex, which are critical for mood regulation [15]. Similar mechanisms are implicated in anxiety disorders and schizophrenia [3].
- Autoimmune and Inflammatory Diseases: Chronic stress leads to HPA axis dysregulation, characterized by impaired feedback, glucocorticoid receptor resistance, and paradoxical cortisol output, which fosters a pro-inflammatory state [7]. This immune imbalance weakens protective mechanisms and shifts the immune response toward autoimmunity, with evidence linking persistent HPA dysfunction to diseases like rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis [7].
- Cardiometabolic Diseases: Programming that results in elevated cortisol can promote the development of hypertension, obesity, insulin resistance, and metabolic syndrome through cortisol's effects on appetite, fat deposition, glucose metabolism, and vascular function [11] [13] [12].
The evidence is compelling that the HPA axis is a key facilitator of the link between early-life adversity and adult disease. Understanding the mechanisms of developmental programming, including the critical windows and the role of the maternal-placental-fetal unit, provides powerful insights for preventive medicine. Future research should focus on multi-omics approaches to integrate genomic, epigenomic, transcriptomic, and proteomic data from longitudinal cohorts, which will help delineate precise biomarkers of risk and resilience [7]. A major unanswered question is the reversibility of HPA alterations, prompting investigation into interventions—ranging from nutritional supplements and probiotics to psychological support for mothers—that could attenuate the lifelong effects of adverse developmental programming [11] [7]. Ultimately, identifying individuals with programmed HPA axis dysregulation early in life could allow for targeted interventions to improve long-term health trajectories.
The hypothalamic-pituitary-adrenal (HPA) axis represents a primary neuroendocrine system governing the physiological response to stress, integrating neural and hormonal signals to maintain homeostasis under challenging conditions. This sophisticated circuitry coordinates adaptive behavioral and physiological responses through the precise regulation of corticotropin-releasing hormone (CRH), arginine vasopressin (AVP), and glucocorticoids. The HPA axis operates as a coordinated functional system wherein CRH and AVP are frequently secreted together and closely cooperate in regulating stress responses, blood pressure, metabolism, and behavior [16]. The fundamental importance of this system is evident in its requirement for stress adaptation and survival, though its dysregulation contributes significantly to numerous pathological conditions spanning psychiatric, metabolic, cardiovascular, and immune disorders [1] [17].
At its core, the HPA axis functions as a neuroendocrine cascade wherein corticotrophin-releasing hormone (CRH) serves as the principal hypothalamic regulator under basal conditions and in response to most acute stressors [18]. CRH, a 41-amino acid peptide produced primarily in the parvocellular neurons of the paraventricular nucleus (PVN) of the hypothalamus, is released into the pituitary portal system upon stress exposure [19]. It stimulates adrenocorticotropic hormone (ACTH) secretion from anterior pituitary corticotrophs through activation of CRH receptor type 1 (CRHR1), a G-protein-coupled membrane receptor [18]. Arginine vasopressin (AVP), co-expressed in many CRH neurons, acts synergistically with CRH to potentiate ACTH release, primarily through V1b receptors [16] [18]. This coordinated peptide signaling ensures robust ACTH secretion, which subsequently stimulates glucocorticoid production (cortisol in humans, corticosterone in rodents) from the adrenal cortex [1].
Table 1: Core Components of the HPA Axis Neuroendocrine Circuitry
| Component | Primary Site of Synthesis | Key Receptors | Major Functions |
|---|---|---|---|
| CRH | Parvocellular PVN neurons | CRHR1 | Principal stimulator of ACTH secretion; coordinates behavioral stress response |
| AVP | Parvocellular PVN neurons (co-localized with CRH) | V1b | Potentiates CRH-induced ACTH release; important for sustained stress response |
| ACTH | Anterior pituitary corticotrophs | MC2R (adrenal) | Stimulates glucocorticoid synthesis and secretion from adrenal cortex |
| Glucocorticoids | Adrenal cortex | GR, MR | Metabolic adaptation, immune modulation, negative feedback on HPA axis |
The critical regulatory feature of the HPA axis is the glucocorticoid-mediated negative feedback system, wherein elevated circulating glucocorticoids act at multiple levels (hippocampus, hypothalamus, pituitary) to suppress further CRH and ACTH release, thus limiting the stress response and preventing excessive activation [1] [18]. This feedback occurs through two primary corticosteroid receptors: the high-affinity mineralocorticoid receptor (MR) and the lower-affinity glucocorticoid receptor (GR) [18]. The balance between these regulatory components determines HPA axis set-point and stress responsiveness, with dysregulation contributing to hypercortisolemia associated with numerous stress-related diseases and age-related pathology [18].
Molecular Signaling Pathways and Mechanisms
Genomic and Non-genomic Signaling Mechanisms
The signaling pathways governing CRH, AVP, and glucocorticoid interactions operate across multiple temporal domains through both genomic and non-genomic mechanisms. Glucocorticoid signaling is mediated through genomic and non-genomic receptors located in cellular membranes and intracellular compartments [16]. The genomic effects involve corticosteroid receptors belonging to the nuclear receptor superfamily of transcription factors that modulate transcriptional processes through direct binding to glucocorticoid response elements (GRE) or mineralocorticoid response elements (MRE) in DNA [16]. The GR is a 97 kDA protein encoded by the NR3C1/Nr3c1 gene that cooperates with several co-regulators, including steroid receptor coactivators (SRCs) [16].
The CRH gene promoter regulation involves complex interactions with glucocorticoids and cAMP pathways. The human CRH promoter does not contain a consensus glucocorticoid regulatory element (GRE), but does possess a negative GRE (nGRE) that mediates, in part, the inhibition of CRH promoter activity by glucocorticoids [20]. Additionally, cAMP stimulates the CRH promoter through both the consensus cAMP response element (CRE) and a previously unrecognized caudal type homeobox response element (CDXRE) [20]. Glucocorticoid-mediated repression of cAMP-stimulated CRH promoter activity involves interactions between the CRE and the upstream nGRE, demonstrating the intricate cross-talk between these signaling pathways [20].
Table 2: Key Signaling Pathways in HPA Axis Regulation
| Signaling Pathway | Key Elements | Biological Effect | Time Domain |
|---|---|---|---|
| CRH/CRHR1 | Gαs-coupled, adenylate cyclase, cAMP, PKA | Stimulates POMC transcription and ACTH secretion | Rapid (seconds to minutes) |
| AVP/V1b | Gαq-coupled, phospholipase C, IP3, DAG, PKC | Potentiates CRH effects on ACTH release | Rapid (seconds to minutes) |
| Glucocorticoid Genomic | GR/MR, GRE/MRE, transcriptional regulation | Negative feedback; metabolic and immune programming | Slow (hours to days) |
| Glucocorticoid Non-genomic | Membrane receptors, second messengers | Rapid feedback inhibition | Rapid (seconds to minutes) |
| cAMP-CRH Promoter | CRE, CDXRE, nGRE, AP-1 proteins | Regulates CRH gene expression | Intermediate (hours) |
The cellular excitability of corticotrophs is dynamically regulated through these signaling pathways. Corticotrophs are electrically excitable and fire both spontaneous single-spike action potentials and secretagogue-induced bursting activity, with bursting resulting in greater increases in intracellular calcium and enhanced ACTH secretion [21]. Large-conductance calcium- and voltage-activated potassium (BK) channels are key regulators of this bursting behavior [21]. Glucocorticoids modulate corticotroph excitability through both BK-dependent and BK-independent mechanisms, with pretreatment with 100 nM corticosterone reducing spontaneous activity and preventing the transition from spiking to bursting after CRH/AVP stimulation [21]. This demonstrates how glucocorticoids fine-tune pituitary responsiveness through regulation of electrical activity patterns.
Pathway Integration and Cross-Talk
The integration of CRH, AVP, and glucocorticoid signaling occurs through complex cross-talk mechanisms at multiple levels. Vasopressin interacts with the HPA axis at various levels—in hypothalamic nuclei affecting CRH release, in the pituitary gland enhancing ACTH release, and in the adrenal glands modulating steroid hormone action [16]. These interactions are facilitated by positive and negative feedback between specific components of the HPA system with engagement of other neurotransmitting and neuropeptidergic pathways [16]. Importantly, the cooperation between AVP and steroid hormones may be affected by cellular stress combined with hypoxia, and by metabolic, cardiovascular, and respiratory disorders [16].
The glucocorticoid feedback mechanism plays an essential role in regulating CRH production and limiting stress responses. The central sensors for this feedback are MR and GR receptors expressed in the brain and pituitary corticotrophs [18]. GRs are distributed throughout the brain but are most concentrated in hypothalamic neurons and corticotrophs, while MRs are present in the hypothalamus and most abundant in the hippocampus [18]. This receptor distribution creates a tiered feedback system wherein MRs primarily regulate basal HPA tone, while GRs mediate stress-induced feedback, allowing for precise control of HPA axis activity across varying conditions.
Experimental Approaches and Methodologies
Electrophysiological Assessment of Corticotroph Activity
The electrophysiological properties of corticotrophs can be investigated using sophisticated techniques including perforated patch-clamp recordings and dynamic clamp technology. In one comprehensive approach, corticotroph cells are acutely isolated from male mice (aged 2-5 months) constitutively expressing green fluorescent protein under the control of the proopiomelanocortin promoter, allowing for specific identification of corticotrophs [21]. Cells are cultured on coverslips in serum-free media and recordings are obtained 24-96 hours after isolation using the perforated patch mode of the whole-cell patch clamp technique with amphotericin B [21].
For electrophysiological recordings, the standard bath solution contains (in mM): 140 NaCl, 5 KCl, 2 CaCl2, 0.1 MgCl2, 10 HEPES, and 10 glucose (pH 7.4, 300 mOsmol/L). The standard pipette solution contains (in mM): 10 NaCl, 30 KCl, 60 K2SO4, 1 MgCl2, 10 HEPES, 10 glucose, and 50 sucrose (pH 7.2, 290 mOsmol/L) [21]. Recordings are performed at room temperature to facilitate stable recordings, with patch pipettes fabricated from borosilicate glass with resistances typically between 2-3 MΩ. A gravity-driven perfusion system is used to apply drugs with a flow rate of 1-2 mL/min to minimize flow-induced artifacts [21].
The dynamic clamp technique provides a powerful method to investigate the role of specific ion channels in regulating electrical activity. This technique allows investigators to add or subtract specific ionic currents in real-time during electrophysiological recordings. In corticotroph studies, researchers have used dynamic clamp to demonstrate that CRH-induced bursting can be switched to spiking by subtracting a fast BK current, whereas addition of a fast BK current can induce bursting in corticosterone-treated cells [21]. This approach has been instrumental in establishing that glucocorticoids modulate corticotroph excitability through both BK-dependent and BK-independent mechanisms.
Molecular and Genetic Approaches
Promoter analysis techniques have been essential for elucidating the molecular mechanisms governing CRH gene regulation. Studies utilizing the mouse corticotroph cell line AtT20 have revealed complex interactions between glucocorticoids and cAMP in regulating CRH promoter activity [20]. Experimental approaches include subcloning CRH 5'-flanking DNA sequence into promoterless luciferase reporter vectors, creating serial 5' deletions of the CRH promoter region, and introducing specific point mutations to identify functional response elements [20].
For CRH promoter studies, the human CRH genomic clone is subcloned into promoterless Photinus (firefly) luciferase reporter vectors [20]. Transient transfections are performed using calcium phosphate precipitation in AtT20 cells, with cotransfection with a Renilla luciferase expression vector to serve as an internal control for transfection efficiency [20]. Cells are typically treated with test substances for 6-8 hours before lysis and luciferase activity measurement using dual-luciferase assays. This approach has identified that cAMP stimulates the CRH promoter through both the consensus CRE and a novel CDXRE, while glucocorticoid-mediated inhibition involves interactions between the CRE and an upstream nGRE [20].
Genetic mouse models have provided significant insights into HPA axis function. Corticotroph-specific BK channel knockout mice (BK−/−) have revealed that glucocorticoids can inhibit excitability through BK-independent mechanisms to control spike frequency [21]. Similarly, CRF knockout mice show impaired adrenal responses to various acute stressors, confirming CRH's critical role in stress-induced ACTH release [19]. These genetic approaches, combined with electrophysiological and molecular techniques, provide a comprehensive toolkit for dissecting the neuroendocrine circuitry governing stress responses.
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents for HPA Axis Investigation
| Reagent/Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| Cell Models | AtT20 mouse corticotroph cell line | CRH promoter analysis; regulation of POMC expression | In vitro studies of gene regulation [20] |
| Animal Models | CRF knockout mice; BK-POMC-GFP mice | Genetic dissection of HPA axis components | Electrophysiology, stress response testing [21] [19] |
| Peptides/Reagents | CRH, AVP, Corticosterone, Dexamethasone | Receptor activation; stress axis modulation | In vitro and in vivo HPA axis challenge studies [21] [20] |
| Promoter Constructs | CRH-luciferase reporters (CRH-663, CRH-433, etc.) | Analysis of promoter regulation and response elements | Luciferase reporter assays [20] |
| Electrophysiology | Amphotericin B, Dynamic clamp systems | Corticotroph electrical activity recording | Perforated patch-clamp recordings [21] |
Visualization of Neuroendocrine Circuitry
Core HPA Axis Signaling Pathway
Figure 1: Core HPA Axis Signaling and Feedback Pathways. This diagram illustrates the integrated neuroendocrine circuitry involving CRH, AVP, and glucocorticoid signaling. The pathway initiates with stressor detection, leading to CRH and AVP co-release from paraventricular nucleus neurons into the pituitary portal system. These peptides stimulate ACTH secretion from anterior pituitary corticotrophs, which subsequently drives glucocorticoid production from the adrenal cortex. Glucocorticoids complete the circuit through negative feedback mediated by GR and MR receptors at multiple levels, including the hypothalamus and pituitary.
Cellular Signaling and Feedback Mechanisms
Figure 2: Cellular Signaling and Regulatory Mechanisms. This diagram details the intracellular signaling pathways in corticotrophs, highlighting the convergence of CRH and AVP signaling on cAMP production, leading to POMC transcription and ACTH secretion through PKA and CREB activation. Glucocorticoid feedback occurs through genomic mechanisms via GR and MR receptors, as well as non-genomic modulation of BK channels that regulate electrical activity patterns. The BK channel regulation represents a key mechanism whereby glucocorticoids fine-tune corticotroph responsiveness.
The intricate neuroendocrine circuitry involving CRH, AVP, and glucocorticoid signaling represents a sophisticated system for maintaining homeostasis under stress conditions. The functional coordination between these components operates as an integrated AVP-HPA system, with vasopressin interacting with the HPA axis at multiple levels through regulation of CRH release, ACTH secretion, and steroid hormone action [16]. Understanding these interactions at molecular, cellular, and systems levels provides crucial insights for developing novel therapeutic strategies targeting stress-related disorders.
The translational implications of this research are substantial, given that dysregulation of the HPA axis contributes to numerous pathological conditions including depression, anxiety, metabolic syndrome, and cardiovascular diseases [16] [17]. Emerging evidence suggests that central and peripheral interactions between AVP and steroid hormones are reprogrammed in cardiovascular and metabolic diseases, with these rearrangements exerting either beneficial or harmful effects depending on context [16]. Furthermore, the demonstration that glucocorticoids modulate corticotroph excitability through both BK-dependent and BK-independent mechanisms reveals potential targets for therapeutic intervention [21].
Future research directions should focus on elucidating the tissue-specific regulation of these signaling pathways, particularly given evidence that glucocorticoids can exert stimulatory or inhibitory effects on CRH gene expression depending on cellular context [20]. Additionally, greater understanding of how these neuroendocrine circuits are reprogrammed in disease states may yield novel approaches for restoring homeostasis. The continued development of sophisticated experimental approaches, including dynamic clamp electrophysiology, genetic models, and promoter analysis techniques, will be essential for advancing our understanding of this critical neuroendocrine circuitry and its implications for human health and disease.
{c#introduction}
Cross-Talk with the Hypothalamic-Pituitary-Gonadal (HPG) Axis: Stress-Reproduction Interfaces
The hypothalamic-pituitary-adrenal (HPA) axis is the body's central neuroendocrine system for responding to stress, culminating in the release of cortisol. In parallel, the hypothalamic-pituitary-gonadal (HPG) axis is the primary regulator of reproductive function, governing the secretion of sex steroids such as testosterone, estrogen, and progesterone. These two systems do not operate in isolation; they engage in a complex, bidirectional crosstalk that is crucial for maintaining homeostasis. Activation of the HPA axis, particularly when chronic, can significantly suppress the reproductive axis. This interface, often described as a stress-reproduction interface, represents a critical adaptive mechanism where the body prioritizes survival over reproductive investment during challenging conditions. Understanding the physiological basis of this interaction, the experimental methods for its study, and the resulting molecular pathways is fundamental to research in stress neuroendocrinology and has profound implications for drug development in areas of stress-related reproductive disorders and infertility [22] [23] [24].
Physiological Basis of HPA-HPG Axes Interaction
The crosstalk between the stress and reproductive axes occurs at multiple levels, from the central nervous system to the peripheral gonads, through hormonal, neural, and intracellular signaling pathways.
Central Neuroendocrine Suppression
At the central level, the primary point of interaction is the suppression of the HPG axis's master regulator, gonadotropin-releasing hormone (GnRH). The stress-induced release of corticotropin-releasing hormone (CRH) from the hypothalamus directly inhibits the pulsatile secretion of GnRH from hypothalamic neurons [25] [24]. This suppression is further mediated by the elevated levels of glucocorticoids (e.g., cortisol) that result from HPA axis activation. Reduced GnRH pulsatility leads to diminished release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the anterior pituitary, which in turn results in suppressed gonadal steroidogenesis and ovulation or spermatogenesis [23] [25]. Furthermore, kisspeptin, a potent stimulator of GnRH neurons, is also suppressed by stress and glucocorticoids, providing another critical pathway for central reproductive inhibition [24].
Peripheral and Molecular Pathways
Beyond the brain, significant interactions occur at the gonadal level. Glucocorticoid receptors are expressed in the ovaries and testes, and high cortisol levels can directly blunt gonadal response to LH and FSH, inhibiting the production of sex steroids like estrogen, progesterone, and testosterone [23]. A key molecular phenomenon is the "cortisol steal" or pregnenolone steal, where the shared precursor, pregnenolone, is shunted away from the synthesis of sex steroids towards the increased production of cortisol in the adrenal cortex under chronic stress, leading to a relative deficiency in progesterone and other downstream reproductive hormones [25].
The autonomic nervous system provides another interface. Stress activates the sympathetic nervous system, which directly innervates the ovaries. Norepinephrine release from these sympathetic terminals can alter follicular development and steroidogenesis, and chronic activation is implicated in conditions like polycystic ovarian syndrome (PCOS) [23]. Finally, the gut-brain axis contributes to this interplay; stress-induced dysbiosis and increased gut permeability can lead to systemic inflammation, which further exacerbates HPA axis dysregulation and negatively impacts reproductive tissues, influencing conditions like endometriosis and PCOS [15] [25].
Experimental Evidence and Research Data
The theoretical framework of HPA-HPG crosstalk is supported by a body of experimental evidence from both animal and human studies, which also reveals a nuanced picture depending on the nature and duration of the stressor.
Table 1: Summary of Key Experimental Findings on Stress-HPG Axis Interactions
| Study Type / Model | Key Experimental Findings | Implications for HPG Function |
|---|---|---|
| Chronic Stress (Animal Models) [23] [24] | Inhibition of GnRH pulsatility; reduced LH/FSH secretion; decreased testosterone, estrogen, and progesterone; suppression of kisspeptin. | Leads to impaired fertility, disrupted estrous cycles, anovulation, and poor reproductive outcomes. |
| Acute Psychosocial Stress (Human Experimental) [26] | Meta-analysis of 21 studies (N=881) shows a stimulatory effect on testosterone, progesterone, and estradiol levels in response to acute laboratory stressors. | Suggests acute stress may transiently stimulate, not inhibit, HPG activity in humans, highlighting a key difference from chronic stress effects. |
| Maternal Separation (Rat Model) [23] | Produced sexually dimorphic effects on reproductive behavior; longer mount/latency times in males, altered maternal programming of reproductive strategy in females. | Early-life stress programs adult sexual behavior and HPG axis set-points via epigenetic and organizational mechanisms. |
| Sympathetic Denervation (Rat Ovarian) [23] | Inhibition of follicular growth following ovarian denervation; norepinephrine facilitates follicular development. | Demonstrates a critical role for direct sympathetic neural input in regulating ovarian function outside classic HPA axis. |
Methodological Protocols for Key Findings
The evidence summarized in Table 1 is derived from rigorous experimental protocols. A standard method for investigating acute stress in humans is the use of standardized acute laboratory stressors, such as the Trier Social Stress Test (TSST). This protocol typically involves a brief preparation period followed by a mock job interview and mental arithmetic task in front of an audience. Saliva or blood samples are collected at baseline, immediately post-stress, and at several time points during recovery (e.g., +10, +20, +30, +60 mins) to measure the dynamic response of gonadal steroids (testosterone, estradiol, progesterone) and cortisol [26].
In animal models, the Maternal Separation (MS) protocol is a classic early-life stress paradigm. In rodents, pups are separated from the dam for periods of 3-8 hours per day during the first two postnatal weeks. Control litters are either left completely undisturbed or subjected to brief handling. The long-term effects on reproductive physiology and behavior, including lordosis quotient, mount latency, and hormone receptor expression in the brain (e.g., ERα in the hypothalamus), are then assessed in adulthood [23].
To elucidate the role of direct sympathetic input to the gonads, the superior ovarian nerve denervation model is used. In rats or mice, this involves surgical transection or chemical ablation of the nerves in the suspensory ligament that innervate the ovary. The functional outcomes, such as follicular development, steroid hormone output, and the incidence of cystic structures, are compared between denervated and sham-operated control animals [23].
Signaling Pathways and Neuroendocrine Circuits
The following diagrams, generated using Graphviz DOT language, illustrate the core signaling pathways and neuroendocrine circuits that mediate the crosstalk between the stress and reproductive axes.
Diagram 1: Central & Peripheral HPA-HPG Cross-Talk
(Central & Peripheral HPA-HPG Cross-Talk)
Diagram 2: Experimental Stress-Reproduction Workflow
(Experimental Stress-Reproduction Workflow)
The Scientist's Toolkit: Research Reagent Solutions
To effectively investigate the HPA-HPG axis crosstalk, researchers rely on a suite of specific reagents, assays, and molecular tools. The following table details key resources essential for experiments in this field.
Table 2: Essential Research Reagents and Materials for HPA-HPG Axis Studies
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| Corticotropin-Releasing Hormone (CRH) | Used to directly stimulate the HPA axis in vivo or in vitro to study downstream effects on HPG function. | Often administered intracerebroventricularly (ICV) in animal models; specific agonists/antagonists (e.g., CRH type 1 receptor antagonists) are used for mechanistic studies. |
| Kisspeptin Agonists/Antagonists | To probe the role of the kisspeptin system in mediating stress effects on GnRH neurons. | e.g., kisspeptin-10 (KP-10) as an agonist; peptide antagonists like p271 used to block kisspeptin receptor (KISS1R) signaling [24]. |
| Enzyme Immunoassays (EIA) & Radioimmunoassays (RIA) | For the precise quantification of hormone levels in serum, plasma, saliva, and tissue culture media. | Widely used for measuring Cortisol, ACTH, Testosterone, Estradiol, Progesterone, LH, and FSH. |
| Glucocorticoid Receptor (GR) Antagonists | To block glucocorticoid signaling and isolate its specific effects in the crosstalk mechanism. | e.g., Mifepristone (RU-486); used in vivo or in cell culture to determine GR-dependent pathways. |
| qPCR Assays & Antibodies for IHC | For molecular analysis of gene and protein expression in neural and reproductive tissues. | Target genes: CRH, AVP, GnRH, Kiss1, POMC, steroidogenic enzymes (e.g., CYP19A1). Antibodies for localization of proteins like ERα, GR, CRH receptors [23]. |
| Stereotaxic Surgery Equipment | For precise cannulation and microinjection of reagents into specific brain nuclei in rodent models. | Used to target the paraventricular nucleus (PVN), arcuate nucleus (where kisspeptin neurons reside), or median eminence. |
The intricate cross-talk between the HPA and HPG axes is a cornerstone of the body's adaptive response to environmental challenges, ensuring that resources are allocated towards survival at the potential cost of immediate reproductive investment. The mechanistic insights, derived from both animal and human studies, reveal a multi-layered interaction involving central neuroendocrine suppression, peripheral gonadal effects, and autonomic nervous system involvement. For researchers and drug development professionals, a deep understanding of these pathways—including the roles of CRH, glucocorticoids, kisspeptin, and sympathetic signaling—is paramount. Future therapeutic strategies for stress-induced reproductive dysfunction may hinge on targeted interventions that reset this critical neuroendocrine dialogue, whether through novel small molecules, neuromodulation, or lifestyle interventions that address the root causes of HPA axis dysregulation.
The gut-brain axis represents one of the most significant paradigms in modern neurobiology, forming a complex, bidirectional communication network that integrates gastrointestinal function with central nervous system activity. Within this framework, the hypothalamic-pituitary-adrenal (HPA) axis—the body's primary neuroendocrine stress response system—engages in continuous crosstalk with the gut microbiota. This interaction is mediated through multiple signaling pathways including neural, endocrine, immune, and metabolic routes [27]. The microbial ecosystem inhabiting the gastrointestinal tract, comprising approximately 100 trillion microorganisms, possesses a genetic potential that vastly exceeds the human genome, positioning it as a powerful environmental factor capable of influencing host physiology and stress responsiveness throughout the lifespan [28] [29].
Understanding the mechanistic basis of microbiota-HPA axis interactions is crucial for stress research and therapeutic development. Evidence from germ-free (GF) animal models demonstrates that the absence of gut microbiota leads to altered stress responses, neurotransmitter levels, and neurodevelopment, which can be partially restored through microbial colonization [30]. Furthermore, clinical observations reveal that disorders such as depression and irritable bowel syndrome (IBS) frequently present with concurrent dysregulation of both the HPA axis and gut microbiota, suggesting a shared pathophysiology [28]. This whitepaper synthesizes current evidence on the communication pathways between gut microbiota and HPA function, with emphasis on mechanistic insights, experimental approaches, and implications for neuroendocrine-related disorders.
Core Communication Pathways in the Microbiota-Gut-Brain Axis
The microbiota-gut-brain axis (MGBA) operates through an integrated network of parallel communication pathways that enable bidirectional information flow between gut microbes and the brain. These pathways collectively regulate HPA axis activity through distinct but interconnected mechanisms.
Neural Pathways
The vagus nerve serves as the most direct neural connection between the gut and brain, with various receptors on vagal afferents sensing and transmitting signals from the gut to the brain [31]. This nerve affects CNS reward neurons and influences mood and behavior [31]. Additionally, the enteric nervous system (ENS) forms a complex intrinsic neural network within the gastrointestinal wall that communicates with the CNS through intestinofugal neurons and vagal afferent pathways [32] [31]. Microbial metabolites including short-chain fatty acids (SCFAs) and neurotransmitters can directly stimulate these neural pathways to modulate brain function and HPA axis activity [33].
Endocrine and Neuroendocrine Pathways
The HPA axis itself functions as a central neuroendocrine pathway within the MGBA. In response to stress, the hypothalamus releases corticotropin-releasing factor (CRF), which triggers pituitary secretion of adrenocorticotropic hormone (ACTH), ultimately stimulating glucocorticoid (cortisol in humans, corticosterone in rodents) release from the adrenal cortex [28]. Gut microbes can influence this cascade through multiple mechanisms, including the production of neuroactive compounds (GABA, serotonin, dopamine) and modulation of gut hormones that circulate to affect brain function [27] [33]. Additionally, glucocorticoids can directly influence gut microbiota composition by altering gut transit time, intestinal permeability, and nutrient availability [29].
Immune and Inflammatory Pathways
The immune system serves as a critical intermediary in gut-brain communication. Gut microbes regulate the development and function of both mucosal and systemic immunity through metabolites such as SCFAs, tryptophan derivatives, and secondary bile acids [30]. Microbial-associated molecular patterns (MAMPs) including lipopolysaccharide (LPS) and peptidoglycan can translocate across compromised intestinal barriers and activate pattern recognition receptors (e.g., Toll-like receptors), triggering neuroinflammatory responses that modulate HPA activity [28] [30]. Proinflammatory cytokines and prostaglandins generated through these mechanisms represent potent activators of the HPA axis [28].
Metabolic Pathways
Gut microbiota produce a diverse array of microbial metabolites that systemically influence host physiology. Short-chain fatty acids (butyrate, acetate, propionate) derived from dietary fiber fermentation demonstrate particularly wide-ranging effects, serving as histone deacetylase (HDAC) inhibitors, G-protein coupled receptor (GPCR) ligands, and modulators of neuroinflammation and blood-brain barrier integrity [34] [33]. Other microbial metabolites including bile acids, tryptophan catabolites, and neurotransmitters additionally contribute to the metabolic regulation of HPA function [27] [30].
Table 1: Primary Communication Pathways in the Microbiota-Gut-Brain Axis
| Pathway | Key Components | Mechanism of HPA Axis Modulation |
|---|---|---|
| Neural | Vagus nerve, Enteric Nervous System (ENS) | Direct neural signaling from gut to brain; microbial metabolites activate vagal afferents [27] [31] |
| Endocrine/Neuroendocrine | HPA axis, Gut hormones, Microbial neurotransmitters | Glucocorticoid feedback; microbial production of neuroactive compounds (GABA, serotonin, dopamine) [27] [33] |
| Immune | Cytokines, MAMPs (LPS, peptidoglycan), TLRs | Immune activation and neuroinflammation; proinflammatory cytokines as HPA activators [28] [30] |
| Metabolic | SCFAs, Bile acids, Tryptophan metabolites | Epigenetic regulation (HDAC inhibition); receptor activation (GPCRs); barrier integrity modulation [34] [30] |
Figure 1: Multidirectional Communication Pathways Linking Gut Microbiota to HPA Axis Function
Key Microbial Metabolites Regulating HPA Activity
Gut microbiota produce a diverse array of bioactive metabolites that systemically influence host physiology, with several demonstrating significant effects on HPA axis regulation. These microbial-derived compounds function through distinct molecular mechanisms to modulate neuroendocrine stress responses.
Short-Chain Fatty Acids (SCFAs)
Butyrate, acetate, and propionate represent the most extensively studied microbially-derived metabolites with HPA-modulating properties. These SCFAs are produced primarily through bacterial fermentation of dietary fiber in the colon and exhibit multiple mechanisms of action [33]. Butyrate in particular functions as a potent histone deacetylase (HDAC) inhibitor, enabling epigenetic regulation of gene expression in stress-responsive brain regions [34] [33]. SCFAs also activate G-protein coupled receptors (GPR41, GPR43, GPR109a) expressed on enteroendocrine cells, immune cells, and peripheral neurons, influencing inflammatory pathways and neurotransmitter release [30]. Additionally, SCFAs contribute to maintenance of intestinal barrier integrity and blood-brain barrier function, indirectly modulating HPA axis activity by limiting translocation of inflammatory mediators [31]. Under acute stress conditions, SCFA levels are frequently reduced, associated with increased inflammation, gut permeability, and alterations in brain function and mood [34].
Neuroactive Metabolites and Neurotransmitters
Gut microbiota significantly influence central neurotransmitter systems through direct production and precursor modulation. Gamma-aminobutyric acid (GABA), the primary inhibitory neurotransmitter in the CNS, is produced by various bacterial species including Lactobacillus and Bifidobacterium [34] [33]. Similarly, catecholamines (dopamine, norepinephrine) are produced by Escherichia, Bacillus, and Proteus species, with levels increasing during acute stress to mediate physiological stress responses [34]. Perhaps most significantly, gut microbiota regulate serotonin biosynthesis, with approximately 90% of the body's serotonin produced by enterochromaffin cells in response to microbial metabolites [33]. Tryptophan availability—the precursor to serotonin—is directly influenced by gut microbes, with acute stress reducing tryptophan levels and shifting metabolism toward the kynurenine pathway, resulting in neuroactive metabolites that influence mood and cognition [34].
Immune-Active Microbial Molecules
Lipopolysaccharide (LPS), a component of the outer membrane of Gram-negative bacteria, represents a potent activator of inflammatory signaling that can influence HPA axis activity. Under conditions of increased intestinal permeability, LPS translocates into systemic circulation and triggers immune activation through Toll-like receptor 4 (TLR4), leading to production of proinflammatory cytokines that stimulate HPA activity [28]. Similarly, bacterial peptidoglycan can translocate into the brain and activate pattern recognition receptors (Nod1), influencing brain development and behavior [28]. These microbial-associated molecular patterns establish a direct link between gut microbiota composition, immune activation, and neuroendocrine function.
Table 2: Key Microbial Metabolites Regulating HPA Axis Function
| Metabolite | Producing Bacteria | Mechanism of Action | Impact on HPA Axis |
|---|---|---|---|
| Butyrate | Faecalibacterium, Ruminococcus, Lactobacillus | HDAC inhibition; GPCR activation; barrier integrity [34] [33] | Reduced under acute stress; anti-inflammatory; epigenetic regulation [34] |
| GABA | Lactobacillus, Bifidobacterium, Bacteroides | Primary inhibitory neurotransmitter; reduced neuronal excitability [34] [33] | Promotes relaxation; reduced stress responsivity; alterations linked to anxiety [34] |
| Serotonin | Precursor regulation by Bacteroides, Clostridium, Enterococcus [34] | Tryptophan metabolism; mood, sleep, emotional regulation [33] | 90% gut-derived; reduced during stress; impacts mood and gut motility [34] [33] |
| Catecholamines | Escherichia, Bacillus, Proteus [34] | Dopamine, norepinephrine, epinephrine synthesis; reward, motivation, alertness [34] [33] | Increased during acute stress; mediates physiological stress responses (heart rate, blood pressure) [34] |
| Lipopolysaccharide (LPS) | Gram-negative bacteria (Escherichia, Bacteroides) [28] | TLR4 activation; proinflammatory cytokine production; immune activation [28] [30] | Potent HPA activator; linked to neuroinflammation and stress susceptibility [28] |
Experimental Models and Methodological Approaches
Research investigating microbiota-HPA axis interactions employs a diverse array of experimental models and methodological approaches, each offering distinct advantages for elucidating specific aspects of this complex relationship.
Germ-Free Animal Models
Germ-free (GF) mice, raised in completely sterile isolators without any microorganisms, represent a foundational model for investigating microbiota-HPA axis interactions. These animals exhibit significant alterations in HPA axis function, including exaggerated corticosterone responses to acute stress compared to conventionally colonized counterparts [28] [30]. The HPA axis hyperactivity observed in GF mice can be normalized by microbial colonization early in life, but not in adulthood, highlighting the importance of critical developmental windows for microbiota-HPA programming [28]. GF models additionally demonstrate immune system abnormalities, including underdeveloped mucosal lymphoid structures, reduced secretory immune factors, and decreased numbers of immune cells, which collectively contribute to altered neuroimmune signaling and HPA regulation [30]. The utility of GF models extends to fecal microbiota transplantation (FMT) studies, where colonization with microbiota from diseased or stressed donors can transfer phenotypic traits including HPA dysregulation to recipient animals [28].
Microbiota Manipulation Approaches
Antibiotic-induced microbiota depletion provides a complementary approach to GF models, enabling investigation of microbiota contributions in adult organisms. Studies demonstrate that antibiotic treatment disrupts microbial community structure and diurnal rhythms of corticosterone release, leading to time-of-day-specific impairments in stress responsivity [35]. Probiotic interventions, typically utilizing specific bacterial strains such as Lactobacillus and Bifidobacterium, have been shown to normalize HPA activity and reduce depressive-like behaviors in both animal studies and human clinical trials [32]. For instance, L. reuteri has been identified as a candidate strain for regulating glucocorticoid rhythmicity [35]. Prebiotic administration, involving dietary compounds that selectively stimulate growth of beneficial bacteria, represents a complementary approach for modulating microbiota-HPA communication, primarily through enhancement of SCFA production [34].
Stress Exposure Paradigms
Controlled stress exposure represents an essential methodological component for investigating bidirectional microbiota-HPA interactions. Early life stress models, including maternal separation and limited nesting material, demonstrate that stress during critical developmental windows produces persistent HPA axis dysregulation associated with microbial dysbiosis, increased intestinal permeability, and immune activation [28]. In adult animals, chronic stress paradigms such as social defeat and chronic restraint stress produce robust alterations in gut microbiota composition, typically characterized by reduced abundance of beneficial bacteria (e.g., Lactobacillus) and increased proportion of potentially pathogenic taxa [32]. These stress-induced microbial changes are associated with exacerbated neuroinflammatory responses and altered HPA axis feedback sensitivity. Acute stress models further reveal rapid, stressor-induced changes in microbial community function and metabolite production, including increased catecholamine levels and altered tryptophan metabolism [34].
Figure 2: Experimental Workflow for Investigating Microbiota-HPA Axis Interactions
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Investigating microbiota-HPA axis interactions requires specialized research reagents and methodological approaches spanning microbiology, neuroendocrinology, and immunology. The following table summarizes essential research tools and their applications in this field.
Table 3: Essential Research Reagents and Methodologies for Microbiota-HPA Axis Research
| Research Tool | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Gnotobiotic Models | Germ-free (GF) mice; Humanized microbiota mice [28] [30] | Establish causal relationships between specific microbes/microbial communities and HPA function [28] [30] | Requires specialized sterile isolators; colonization timing critical for developmental studies [28] |
| Probiotic Strains | Lactobacillus spp. (e.g., L. reuteri); Bifidobacterium spp. [32] [35] | Investigate therapeutic modulation of HPA axis; mechanism of action studies [32] [34] | Strain-specific effects; dosage and administration route critical; viability assessment essential [32] |
| Microbiome Sequencing | 16S rRNA gene sequencing; Shotgun metagenomics [36] [33] | Microbial community profiling; functional potential assessment; identification of microbial signatures [36] [33] | Choice of hypervariable region (16S); contamination controls; integration with metabolomic data [36] |
| HPA Axis Assessment | Corticosterone/Cortisol ELISA/RIA; CRF/ACTH immunoassays; Dexamethasone suppression test [28] [32] | Quantify HPA axis activity under basal and stress conditions; feedback sensitivity assessment [28] [32] | Diurnal rhythm considerations; appropriate stress paradigms; sampling time points critical [35] |
| Metabolomic Analysis | LC-MS/MS for SCFAs, neurotransmitters; Targeted metabolomics [34] [33] | Quantify microbial metabolites in gut, blood, brain; metabolic pathway analysis [34] [33] | Sample collection stability; comprehensive coverage; integration with microbial data [34] |
| Immune Profiling | Cytokine multiplex assays; Flow cytometry; TLR signaling assays [28] [30] | Characterize neuroimmune activation; inflammatory mediator quantification [28] [30] | Tissue-specific immune responses; activation states; cell population identification [30] |
Implications for Disease Pathophysiology and Therapeutic Development
Dysregulation of microbiota-HPA axis communication has been implicated in the pathophysiology of multiple neurological, psychiatric, and gastrointestinal disorders, revealing promising avenues for therapeutic intervention.
Stress-Related Psychiatric Disorders
Major depressive disorder is frequently associated with both HPA axis hyperactivity and gut microbial dysbiosis. Individuals with depression demonstrate distinct microbial signatures characterized by reduced abundance of SCFA-producing bacteria, altered tryptophan metabolism, and increased proinflammatory potential [33]. Preclinical studies demonstrate that fecal microbiota transplantation from depressed patients to germ-free rodents can induce depression-like behaviors, supporting a causal role for gut microbes in mood regulation [28]. Similarly, anxiety disorders have been linked to microbiota-HPA axis dysregulation, with probiotic interventions containing Lactobacillus and Bifidobacterium strains demonstrating efficacy in reducing anxiety-like behaviors in both animal models and human populations [32] [33]. The adolescent period represents a particularly sensitive window for microbiota-HPA interactions, with stress during this developmental stage producing enduring effects on frontolimbic circuitry and stress responsiveness [32].
Neurodevelopmental and Neurodegenerative Disorders
Neurodevelopmental disorders including autism spectrum disorder (ASD) are associated with early-life alterations in gut microbiota composition and HPA axis function. Maternal immune activation models demonstrate that prenatal stress can induce microbial dysbiosis in offspring that persists into adulthood, accompanied by social behavior deficits and HPA axis dysregulation [31]. Neurodegenerative disorders including Alzheimer's disease and Parkinson's disease also demonstrate alterations in gut microbiota composition, with animal models suggesting that microbial manipulation can modify disease progression [36] [27]. The mechanisms linking gut microbiota to neurodegeneration likely involve bidirectional communication along the gut-brain axis, with microbial metabolites and immune activation contributing to neuroinflammation and protein aggregation [27].
Therapeutic Implications and Future Directions
The growing understanding of microbiota-HPA axis interactions has stimulated development of novel therapeutic approaches targeting the gut microbiome for neuropsychiatric disorders. Probiotic interventions utilizing specific bacterial strains with neuroactive properties represent a promising strategy for HPA axis modulation, with clinical trials demonstrating beneficial effects on stress responsivity and mood [32] [33]. Prebiotic compounds that selectively enhance growth of beneficial taxa offer a complementary approach, primarily through stimulation of SCFA production [34]. Fecal microbiota transplantation represents a more intensive intervention that has shown efficacy in animal models for transferring behavioral phenotypes, highlighting the potential for microbiome-based therapeutics [28]. Future research directions include development of personalized microbiome-based interventions tailored to individual microbial and immune profiles, identification of microbiome-based biomarkers for stress susceptibility and treatment response, and exploration of dietary interventions designed to optimize microbiota-HPA axis communication [30] [33].
Advanced Assessment Techniques and Therapeutic Targeting of HPA Axis Pathways
The hypothalamic-pituitary-adrenal (HPA) axis serves as the body's primary neuroendocrine stress response system, coordinating adaptive physiological processes to maintain homeostasis. Dysregulation of this axis represents a fundamental mechanism linking chronic stress to various pathological conditions, including major depressive disorder, neurodegenerative diseases, and autoimmune conditions [37] [7] [15]. Biomarker profiling of the HPA axis provides critical insights into these pathological processes by quantifying dynamic changes in hormonal secretions and receptor expression patterns. This technical guide details the core methodologies for comprehensive assessment of cortisol dynamics, corticotropin-releasing hormone (CRH) measurement, and glucocorticoid receptor expression analysis, providing researchers and drug development professionals with standardized approaches for investigating HPA axis function in stress-related research.
The analytical framework for HPA axis biomarker profiling integrates multiple temporal and functional dimensions, from rapid hormonal pulses to long-term receptor adaptations. Cortisol, the primary glucocorticoid in humans, exhibits complex pulsatile secretion patterns that are regulated by the circadian rhythm and stress exposure [37]. Simultaneously, CRH functions as the primary secretagogue driving the HPA axis cascade, while glucocorticoid receptors (GRs) and mineralocorticoid receptors (MRs) mediate the physiological effects of cortisol and execute critical negative feedback mechanisms [37] [38]. The intricate interplay between these components necessitates multidimensional assessment strategies to fully characterize HPA axis dysfunction in pathological states.
Cortisol Dynamics: Quantitative Assessment and Methodologies
Cortisol Biosynthesis and Physiological Regulation
Cortisol biosynthesis follows a carefully orchestrated neuroendocrine cascade beginning with hypothalamic CRH release, which stimulates anterior pituitary production of adrenocorticotropic hormone (ACTH), ultimately prompting adrenal cortisol synthesis and secretion [37]. Approximately 5% of circulating cortisol exists in a free, biologically active form, while the remainder is bound to corticosteroid-binding globulin (80% with high affinity) and albumin (15% with low affinity) [37]. Only free cortisol can enter cells and interact with glucocorticoid receptors, providing feedback inhibition in the hypothalamus and pituitary gland to regulate HPA axis activity [37]. This feedback mechanism is crucial for maintaining physiological equilibrium and becomes dysregulated under conditions of chronic stress.
The circadian rhythm of adrenal glucocorticoid release consists of pulses with varying amplitudes generated by a sub-hypothalamic pulse generator [37]. These oscillating endogenous glucocorticoid signals interact with regulatory systems throughout the HPA axis, including the adrenal gland itself, where a regulatory network can modify pulsatile hormone release [37]. The resulting HPA axis output is a dynamic, oscillating glucocorticoid signal that requires sophisticated decoding at the cellular level. Even slight alterations in this system's dynamics during chronic stress or disease states can significantly impact functional output across multiple tissues, leading to changes in metabolic processes, behavior, mood, and cognition [37].
Methodologies for Cortisol Assessment
Sample Collection and Processing: Cortisol can be measured in multiple biofluids, including serum, plasma, and saliva. For serum cortisol assessment, blood should be collected following an overnight fast, typically between 7:30 and 9:30 AM to account for diurnal variation [39]. Salivary cortisol measurement requires participants to collect samples using salivettes at specified times: upon awakening, 30 minutes after awakening, and before bedtime [39]. Samples should be centrifuged, with saliva supernatant aliquoted and stored at -80°C until assayed. Timing of sample collection should be rigorously documented, with exclusion of samples collected outside predetermined windows (e.g., before 4 AM or after noon) [39].
Analytical Techniques: Common laboratory methods for cortisol quantification include enzyme-linked immunosorbent assay (ELISA) with inter-assay coefficients of variation typically ranging from 3.8% (high concentration) to 8.1% (low concentration) for serum, and 3.75% to 6.41% for salivary cortisol [39]. Emerging technologies aim to enable point-of-care cortisol detection, though most applications remain laboratory-based [40]. For comprehensive assessment, multiple cortisol biomarkers should be calculated:
- Cortisol Awakening Response (CAR): Calculated as the difference between 30-minute post-awakening and awakening salivary cortisol concentrations [39]
- Diurnal Cortisol Slope (DCS): Determined as the difference between evening and awakening salivary cortisol levels [39]
- Total Daily Cortisol (TDC): Computed as the total area under the curve (AUC) for the three daily samples using the trapezoid rule [39]
Table 1: Cortisol Biomarkers and Their Physiological Significance
| Biomarker | Measurement Approach | Physiological Significance | Research Applications |
|---|---|---|---|
| Serum Cortisol (sCOR) | Single morning blood draw | Captures circulating cortisol at specific time point | Diagnostic screening for HPA axis disorders |
| Cortisol Awakening Response (CAR) | Salivary samples at awakening and 30min post | Reflects HPA axis reactivity to morning awakening | Stress reactivity studies, psychiatric disorders |
| Diurnal Cortisol Slope (DCS) | Multiple salivary samples across day | Indicates circadian rhythm integrity | Chronic stress, burnout, metabolic studies |
| Total Daily Cortisol (TDC) | Area under curve from multiple samples | Represents integrated daily cortisol exposure | Cumulative stress load assessment |
Dynamic Testing Protocols
Dexamethasone Suppression Tests: The dexamethasone suppression test, particularly the combined dexamethasone/CRH test (Dex-CRH test), is a valuable tool for investigating HPA axis dysregulation in conditions like major depression [41]. This test involves administration of dexamethasone followed by CRH stimulation to assess feedback sensitivity and pituitary responsiveness. In Cushing disease (pituitary ACTH-secreting adenoma), CRH stimulation typically causes a greater than 35% increase in corticotropin and a greater than 20% rise in cortisol levels, while adrenal tumors or ectopic ACTH-producing tumors show suppressed responses [41].
CRH Stimulation Test: The CRH test evaluates pituitary and adrenal responsiveness. Synthetic ovine CRH is injected intravenously (1 µg/kg body weight or 100 µg total dose) as a bolus over 30 seconds [41]. Blood specimens for ACTH and cortisol analysis are collected at 15 (or 5) and 0 minutes prior to, then at 15, 30, 45, 60, 90, and 120 minutes after CRH administration. Normal findings typically include a peak ACTH level of 10-120 pg/mL (2.2-24 pmol), representing a 35-900% increase from baseline within 10-30 minutes post-injection, and a peak cortisol level of 13-36 µg/dL (360-1000 nmol/L), representing a 20-600% increase within 30-60 minutes [41].
Table 2: Reference Values for CRH Stimulation Test
| Parameter | Baseline | Peak Level | Increase from Baseline | Time to Peak |
|---|---|---|---|---|
| Corticotropin (ACTH) | - | 10-120 pg/mL (2.2-24 pmol) | 35-900% | 10-30 min post-injection |
| Cortisol | - | 13-36 µg/dL (360-1000 nmol/L) | 20-600% | 30-60 min post-injection |
Corticotropin-Releasing Hormone (CRH) Measurement
Preanalytical Considerations for CRH Bioassay
Sample Collection Methodology: For CRH measurement, plasma is generally preferred over serum or whole blood [42]. Collection should utilize EDTA-containing tubes ("lavender top" tubes) to prevent coagulation and preserve analyte integrity. Evans et al. (2001) reported significantly different CRH assay results between plasma and serum samples (46% higher in serum), suggesting that cellular products in serum can render falsely elevated CRH values [42]. Unlike cortisol, CRH production and secretion do not follow a circadian rhythm, particularly during pregnancy where it is continuously produced and released by the placenta in a pulsatile fashion [42]. This characteristic allows researchers flexibility in scheduling sample collection without time-of-day restrictions.
Sample Processing and Storage: Time and temperature critically influence CRH stability. The "gold standard" approach includes chilled centrifugation and preparation of plasma within 2 hours of collection, followed by either immediate assay or frozen storage at -80°C [42]. When immediate processing is not feasible, CRH may remain stable for up to 120 hours in plasma samples maintained continuously at 4°C (standard refrigeration temperature) [42]. However, at elevated temperatures (30°C), CRH stability in plasma decreases dramatically to approximately 18 hours post-collection [42]. For clinical research applications balancing practical constraints with analytical integrity, delayed processing within 12 hours of collection with continuous chilling at 4°C represents an acceptable protocol.
Analytical Approaches and Methodological Challenges
Assay Selection: CRH can be measured using either radioimmunoassay (RIA) or enzyme-linked immunosorbent assay (ELISA) methodologies [42]. Synthetic ovine CRH is typically used in clinical testing as it is equipotent to human CRH but exhibits a more prolonged duration of action [41]. It is important to note that in humans, CRH binds to a plasma CRH-binding protein, which may influence measurement results [41]. Researchers should carefully follow manufacturer protocols from reference laboratories, as unexpected results often stem from deviations from established bioassay procedures [42].
Interpretation of Results: CRH testing has a sensitivity of 86% and specificity of 90% in assessing corticotropin-dependent Cushing syndrome [41]. The test is particularly valuable for differentiating between various forms of adrenal insufficiency:
- Primary adrenal insufficiency: Characterized by high baseline ACTH levels that increase further in response to CRH, while cortisol levels remain low before and after CRH administration [41]
- Secondary (pituitary) adrenal insufficiency: Demonstrates low baseline ACTH levels that do not respond to CRH, with cortisol levels unaffected by CRH stimulation [41]
- Tertiary (hypothalamic) disease: Shows low baseline ACTH levels with exaggerated, prolonged responses to CRH, while serum cortisol levels do not exceed 20 µg/dL [41]
Recent research has identified clinically significant cases where adrenal insufficiency occurs despite preserved ACTH levels within or above the normal range [43]. Gel filtration chromatography has revealed high-molecular-weight ACTH forms in such patients, suggesting altered proopiomelanocortin processing or post-translational modifications that impair ACTH bioactivity [43]. This finding underscores the importance of comprehensive endocrine assessment beyond isolated hormone measurements.
Glucocorticoid Receptor Expression Analysis
Receptor Subtypes and Distribution
Glucocorticoids exert their effects through two primary receptor types: mineralocorticoid receptors (MRs) and glucocorticoid receptors (GRs) [37]. MRs demonstrate a much higher affinity for glucocorticoids and are predominantly concentrated in limbic structures, particularly the hippocampus [37]. In contrast, GRs are distributed throughout the central nervous system and exhibit high affinity only at the peak of the circadian rhythm and immediately following stress exposure [37]. MRs primarily mediate the proactive feedback mode, mediating the inhibitory action of the hippocampus on HPA activity, while GRs mediate the reactive feedback mode under conditions of elevated glucocorticoid levels [37]. This receptor diversity enables sophisticated regulation of HPA axis activity across varying glucocorticoid concentrations.
The critical role of GR signaling in PVN neurons for HPA axis regulation has been demonstrated through sophisticated genetic models. Conditional deletion of GR exon 3 in Sim1-expressing neurons of the hypothalamus (Sim1Cre-GRe3Δ mice) results in 87% GR loss in the PVN, leading to elevated basal and stress-induced corticosterone levels, impaired dexamethasone suppression, increased CRH mRNA in the PVN, and increased basal plasma ACTH levels [38]. These findings establish that loss of PVN GR results in severe HPA axis hyperactivity and a Cushing's syndrome-like phenotype, highlighting the essential role of PVN GR in negative feedback regulation [38].
Methodologies for Receptor Expression Analysis
Immunohistochemistry: For GR protein localization, tissue samples should be collected from anesthetized animals following perfusion with DEPC 1× PBS and 4% DEPC paraformaldehyde [38]. After post-fixing in 4% DEPC PFA overnight, brains are immersed in 70% ethanol and processed for paraffin embedding. Sections are cut at 5-8μm thickness, deparaffinized, and rehydrated before antigen retrieval in 10 mM citrate buffer (pH 6.0) [38]. Blocking should be performed with 3% normal goat serum/0.25% Triton-X-100 in PBS to prevent nonspecific binding. Primary antibodies (e.g., rabbit m20-anti-GR, Santa Cruz Biotechnology sc-1004 at 1:200 dilution) are applied followed by appropriate secondary antibodies (e.g., biotinylated goat antirabbit IgG at 1:250) [38]. Visualization can be enhanced using avidin/biotin complex with cyanine-3 tyramide amplification, with counterstaining using DAPI for nuclear identification.
Genetic Models for Receptor Analysis: Cre-loxP technology enables cell-type-specific deletion of GR isoforms to investigate their functional roles. The Sim1Cre transgenic mouse line drives Cre expression in PVN neurons, allowing recombination of floxed GR alleles [38]. Different deletion strategies target specific functional domains:
- Exon 1C-2 deletion: Removes promoter elements, translation start site, and transcriptional activation domain
- Exon 3 deletion: Removes the zinc finger of the DNA-binding domain [38]
These models demonstrate that deletion efficiency and residual production of truncated GR fragments significantly impact phenotypic outcomes, with exon 3 deletion producing more severe HPA axis dysregulation [38].
Integrated Research Approaches and Applications
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for HPA Axis Biomarker Profiling
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| CRH Formulations | Synthetic ovine CRH, Human CRH | CRH stimulation tests | Ovine CRH has prolonged activity; human CRH not FDA-approved |
| Glucocorticoids | Dexamethasone, Corticosterone | Suppression tests, receptor studies | Dexamethasone used for specific GR activation |
| GR Antibodies | Rabbit m20-anti-GR (sc-1004) | Immunohistochemistry, Western blot | Targets N-terminus of GR |
| Specialized Assays | ELISA kits, RIA kits | Hormone quantification | Consider cross-reactivity with similar molecules |
| Cell Type-Specific Markers | Sim1-Cre transgenic mice | Targeted receptor deletion | Enables PVN-specific GR knockout |
| Sample Collection | EDTA tubes ("lavender top"), Salivettes | Plasma CRH, salivary cortisol | EDTA preserves CRH integrity |
Pathophysiological Applications and Research Insights
Chronic stress leads to profound alterations in HPA axis function, characterized by impaired feedback regulation, glucocorticoid receptor resistance, and paradoxical cortisol dysregulation that fosters a proinflammatory state [7]. This dysregulation promotes cytokine imbalance, weakens protective immune mechanisms, and shifts the immune response toward autoimmunity [7]. Evidence from both human and animal studies associates persistent HPA dysfunction with autoimmune conditions including systemic lupus erythematosus, rheumatoid arthritis, and multiple sclerosis [7]. The relationship between perceived stress and cortisol biomarkers, however, is not always straightforward, with studies showing inconsistent associations between perceived stress scales and cortisol measurements [39].
Animal models have been instrumental in elucidating complex cortisol dynamics during stress, revealing the interplay between physiological, neuroendocrine, and immune factors in the stress response [37]. Research comparing cortisol and corticosterone in rodents found a strong correlation (r = 0.6-0.85) between these hormones across various stress conditions, with corticosterone serving as a more adaptation-related biomarker during chronic stress, while cortisol responds more quickly during severe acute stress [37]. These findings highlight the importance of selecting appropriate biomarkers and model systems for specific research questions.
The gut-brain axis represents another critical pathway interacting with HPA axis function, particularly in depression pathology. Gut dysbiosis can increase intestinal permeability, allowing endotoxins to enter systemic circulation and promote neuroinflammation that alters neurotransmitter production, including serotonin, which is predominantly produced in the gut [15]. This pathway creates a vicious cycle wherein chronic stress alters gut microbiota, which in turn exacerbates HPA axis dysregulation through inflammatory mechanisms [15].
Comprehensive biomarker profiling of cortisol dynamics, CRH measurement, and receptor expression provides invaluable insights into HPA axis function and dysregulation in stress-related pathologies. The methodologies outlined in this technical guide represent current best practices for investigating this complex neuroendocrine system, integrating approaches from basic hormone measurement to sophisticated genetic manipulation models. As research advances, emerging technologies including point-of-care cortisol detection, multi-omics approaches, and refined receptor imaging techniques will further enhance our understanding of HPA axis dynamics. These developments will ultimately facilitate novel therapeutic strategies targeting specific components of HPA axis dysfunction across a spectrum of neurological, psychiatric, and autoimmune conditions.
Genetic and Epigenetic Methodologies for Investigating HPA Axis Regulation
The hypothalamic-pituitary-adrenal (HPA) axis represents the body's primary neuroendocrine stress response system, coordinating physiological adaptations to real or perceived threats through glucocorticoid secretion [1] [44]. Investigation of HPA axis regulation has evolved beyond traditional physiological approaches to incorporate sophisticated genetic and epigenetic methodologies that reveal molecular mechanisms underlying stress vulnerability and resilience [45] [46]. This technical guide provides comprehensive methodologies for investigating HPA axis regulation within contemporary stress research frameworks, emphasizing practical implementation for researchers and drug development professionals.
The HPA axis functions through a cascade beginning with corticotropin-releasing hormone (CRH) release from hypothalamic paraventricular nucleus (PVN) neurons, triggering pituitary adrenocorticotropic hormone (ACTH) secretion, which subsequently stimulates adrenal cortisol production [1] [44]. This system maintains homeostasis through negative feedback mechanisms where glucocorticoids act at brainstem, limbic, and hypothalamic levels to inhibit further CRH neuronal activity [1]. Dysregulation of this finely tuned system contributes to various pathological states, including mood disorders, anxiety disorders, post-traumatic stress disorder (PTSD), and major depressive disorder (MDD) [45] [47] [46].
Table 1: Core Components of the HPA Axis and Their Investigative Significance
| Component | Key Elements | Investigative Significance |
|---|---|---|
| Hypothalamus | Paraventricular Nucleus (PVN), Corticotropin-Releasing Hormone (CRH) neurons | Initiation of stress response; site for genetic/epigenetic regulation of CRH |
| Pituitary | Anterior lobe, Corticotropes, CRH receptors, Proopiomelanocortin (POMC) | ACTH synthesis and secretion; integration of regulatory signals |
| Adrenal | Adrenal cortex, Glucocorticoid synthesis enzymes, Melanocortin 2 receptors (MC2R) | Final output of HPA axis; cortisol/corticosterone production |
| Regulatory Circuits | Hippocampus, Prefrontal Cortex, Amygdala, Brainstem nuclei | Higher-order regulation; negative feedback sites; stress integration |
Genetic Methodologies for HPA Axis Investigation
Genome-Wide Association Studies (GWAS) and Polygenic Risk Scoring
GWAS methodologies enable identification of genetic variants associated with HPA axis dysfunction across stress-related disorders. Current protocols involve large-scale meta-analyses across multiple cohorts to detect single nucleotide polymorphisms (SNPs) with small effect sizes that collectively contribute to HPA-related pathologies [45].
Experimental Protocol: GWAS for HPA Axis Traits
- Cohort Selection: Recruit participants with precise HPA axis phenotyping (diurnal cortisol sampling, dexamethasone suppression test results, psychosocial stress response)
- Genotyping: Utilize high-density SNP arrays (Illumina Infinium Global Screening Array or similar)
- Quality Control: Apply standard filters (call rate >98%, Hardy-Weinberg equilibrium p>1×10⁻⁶, minor allele frequency >1%)
- Imputation: Reference-based imputation using 1000 Genomes Project or TOPMed reference panels
- Association Analysis: Perform linear or logistic regression with appropriate covariates (age, sex, genetic ancestry principals)
- Meta-Analysis: Combine results across cohorts using fixed or random effects models
Recent GWAS have identified HPA-relevant risk loci including HLA-B in PTSD, demonstrating immune-HPA axis interactions [45]. Polygenic risk scores (PRS) aggregate these genetic effects to predict individual differences in stress response, though they typically explain only a small portion of phenotypic variance [45].
Functional Characterization of Risk Loci
Post-GWAS functional characterization aims to bridge statistical associations with biological mechanisms through several approaches:
Expression Quantitative Trait Loci (eQTL) Mapping
- Protocol: Correlate genotype data with gene expression levels from relevant tissues (pituitary, adrenal, or brain regions from post-mortem samples)
- Application: The PTSD-associated SNP rs142174523 was found to regulate expression of 16 genes involved in inflammatory and immune processes [45]
CRISPR-Based Functional Validation
- Protocol: Utilize CRISPR-Cas9 to introduce risk variants in induced pluripotent stem cell (iPSC) models followed by differentiation into hypothalamic neurons or adrenal cortical cells
- Readouts: CRH secretion, glucocorticoid receptor sensitivity, ACTH responsiveness
Table 2: Genetic Methodologies for HPA Axis Investigation
| Methodology | Key Applications | Technical Requirements | Data Outputs |
|---|---|---|---|
| GWAS | Identifying genetic variants associated with HPA axis dysfunction | Large cohorts (>10,000 subjects), High-density genotyping arrays | SNP associations, Genetic loci |
| Polygenic Risk Scoring | Predicting individual stress vulnerability, Gene-environment interactions | Summary statistics from GWAS, Target genotype data | PRS values, Variance explained |
| eQTL Mapping | Linking genetic variants to gene expression | Genotype and RNA sequencing from same tissue | eQTL associations, Candidate genes |
| CRISPR Functional Screening | Validating causal mechanisms, Pathway identification | iPSC models, CRISPR libraries, Differentiation protocols | Functional phenotypes, Pathway analyses |
Epigenetic Methodologies for HPA Axis Investigation
DNA Methylation Profiling
DNA methylation represents the most extensively studied epigenetic mechanism in HPA axis regulation, involving covalent addition of methyl groups to cytosine residues primarily at CpG sites [46]. Methodologies focus on both candidate gene and genome-wide approaches.
Bisulfite Conversion-Based Methods
- Principle: Sodium bisulfite converts unmethylated cytosines to uracils while methylated cytosines remain unchanged, allowing methylation-specific detection
- Whole Genome Bisulfite Sequencing (WGBS): Provides single-base resolution methylation maps across the entire genome
- Reduced Representation Bisulfite Sequencing (RRBS): Cost-effective alternative enriching for CpG-rich regions
- Epigenome-Wide Association Studies (EWAS): Array-based approaches (Illumina EPIC array) assessing ~850,000 CpG sites
Experimental Protocol: EWAS of HPA Axis Dysregulation
- Sample Collection: Obtain target tissue (blood, saliva, or post-mortem brain regions like prefrontal cortex, hippocampus)
- DNA Extraction: Use standardized kits with quality control (A260/A280 ratio, fragment analysis)
- Bisulfite Conversion: Employ commercial kits (Zymo Research EZ DNA Methylation Kit or similar)
- Array Processing: Hybridize to EPIC array following manufacturer protocols
- Quality Control: Check bisulfite conversion efficiency, detection p-values, sample outliers
- Normalization: Apply functional normalization or subset quantile normalization
- Differential Methylation Analysis: Use linear models adjusting for cell type heterogeneity and technical covariates
Key HPA axis genes showing methylation changes in stress-related disorders include glucocorticoid receptor (NR3C1), brain-derived neurotrophic factor (BDNF), FKBP5, and corticotropin-releasing hormone receptor 1 (CRHR1) [46]. Studies demonstrate that early-life stress associates with persistent NR3C1 hypermethylation, impairing negative feedback and promoting HPA axis hyperactivity [46].
Histone Modification Profiling
Histone post-translational modifications (acetylation, methylation, phosphorylation) regulate chromatin accessibility and gene expression in HPA axis pathways [45] [46].
Chromatin Immunoprecipitation Sequencing (ChIP-seq)
- Protocol: Crosslink proteins to DNA, fragment chromatin, immunoprecipitate with histone modification-specific antibodies, sequence bound DNA
- Key Applications: Mapping H3K9me3 depletion at B2 SINE retrotransposons after glucocorticoid exposure [45], profiling histone acetylation changes at stress-responsive gene promoters
Experimental Protocol: ChIP-seq for Glucocorticoid-Induced Histone Changes
- Cell/Tissue Treatment: Expose to glucocorticoids (corticosterone, dexamethasone) or vehicle
- Crosslinking: Use 1% formaldehyde for 10 minutes at room temperature
- Chromatin Shearing: Optimize sonication to achieve 200-500bp fragments
- Immunoprecipitation: Incubate with antibodies against specific modifications (H3K27ac, H3K4me3, H3K9me3)
- Library Preparation: Use sequencing-compatible kits (Illumina TruSeq ChIP Library Preparation Kit)
- Sequencing: Perform on Illumina platform (minimum 20 million reads per sample)
- Bioinformatic Analysis: Align reads, call peaks, identify differential enrichment regions
Non-Coding RNA Profiling
Non-coding RNAs, particularly microRNAs (miRNAs) and long non-coding RNAs (lncRNAs), participate in HPA axis regulation by fine-tuning gene expression [46].
miRNA Sequencing
- Protocol: Extract small RNAs, prepare sequencing libraries, profile expression changes
- Application: Identifying stress-responsive miRNAs that regulate glucocorticoid receptor expression and signaling
Integrated Experimental Designs and Workflows
Longitudinal Stress Paradigms with Multi-Omics Profiling
Comprehensive HPA axis investigation requires integrated approaches capturing dynamic responses across timescales.
Experimental Design: Chronic Stress Trajectories
- Stress Induction: Apply chronic variable stress, social defeat, or early-life stress paradigms in animal models
- Longitudinal Sampling: Collect serial samples (blood, tissue biopsies) across stress exposure and recovery
- Multi-Omics Profiling: Generate parallel genomic (whole genome sequencing), epigenomic (WGBS, ChIP-seq), transcriptomic (RNA-seq), and proteomic data
- Phenotypic Assessment: Measure behavioral (anxiety-, depression-like behaviors), physiological (corticosterone levels, weight), and neuroendocrine (dexamethasone suppression) endpoints
- Data Integration: Employ computational methods (multi-omics factor analysis) to identify coordinated molecular networks
This approach revealed that stress-induced molecular alterations can manifest as vulnerability in one context and resilience in another, supporting the "Three-hit concept for vulnerability and resilience" [45].
Cross-Species Validation Frameworks
Translational HPA axis research requires careful cross-species validation strategies:
Protocol: Cross-Species Epigenetic Conservation
- Identify Orthologous Regions: Map stress-associated epigenetic marks between human and model organisms
- Functional Testing: Manipulate candidate regions in model systems (CRISPR epigenome editing)
- Conservation Assessment: Determine evolutionary conservation of regulatory mechanisms
- Therapeutic Translation: Test epigenetic-targeting compounds in model systems before human trials
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for HPA Axis Genetic/Epigenetic Investigation
| Reagent Category | Specific Examples | Application Notes |
|---|---|---|
| Genotyping Arrays | Illumina Infinium Global Screening Array, PsychArray | Optimized for psychiatric genetics, includes stress-relevant variants |
| Bisulfite Conversion Kits | Zymo Research EZ DNA Methylation Kit, Qiagen EpiTect Fast | Conversion efficiency >99% critical for reliable results |
| Methylation Arrays | Illumina Infinium MethylationEPIC v2.0 | Covers >900,000 CpG sites including enhancer regions |
| ChIP-Grade Antibodies | Diagenode, Abcam, Cell Signaling Technology | Validate for species specificity and application performance |
| Glucocorticoid Receptor Modulators | Dexamethasone, Corticosterone, RU486, CORT113176 | Dose-response curves essential; consider receptor specificity |
| Stress Paradigms | Trier Social Stress Test, Chronic Variable Stress, Social Defeat | Standardize timing, intensity, and context across experiments |
| CRISPR Epigenetic Editors | dCas9-DNMT3A, dCas9-TET1, dCas9-p300 | Targeted methylation/demethylation and acetylation for functional validation |
Signaling Pathways and Experimental Workflows
Genetic and Epigenetic Regulation of HPA Axis Signaling
Figure 1: Genetic and Epigenetic Regulation of HPA Axis Signaling
Integrated Multi-Omics Workflow for HPA Axis Research
Figure 2: Multi-Omics Workflow for HPA Axis Investigation
Data Analysis and Integration Frameworks
Statistical Approaches for Genetic and Epigenetic Data
Analysis of HPA axis genetic and epigenetic data requires specialized statistical approaches:
Polygenic Risk Score Analysis
- Implementation: PRSice-2 or PLINK for calculating polygenic scores
- Covariate Adjustment: Essential to include ancestry principal components
- Interpretation: PRS for PTSD explains ~2-3% of variance in stress-related outcomes [45]
Epigenome-Wide Association Analysis
- Software: minfi, ChAMP, or meffil for EWAS analysis
- Multiple Testing Correction: False discovery rate (FDR <0.05) or Bonferroni correction
- Cell Type Deconvolution: Estimate neuronal/glial proportions in brain tissue using reference datasets
Multi-Omics Integration
- Methods: MOFA+, mixOmics, or Similarity Network Fusion
- Application: Identify coordinated genetic, epigenetic, and transcriptomic changes in HPA axis pathways
Functional Annotation and Pathway Analysis
Prioritized genetic variants and epigenetic marks require functional annotation:
Genomic Context Annotation
- Tools: ANNOVAR, SnpEff, FUMA
- Features: Regulatory elements (enhancers, promoters), chromatin states, evolutionary conservation
Pathway Enrichment Analysis
- Methods: Gene set enrichment analysis (GSEA), over-representation analysis (ORA)
- Databases: GO, KEGG, Reactome, MSigDB Hallmark gene sets
- HPA-Relevant Pathways: Glucocorticoid receptor signaling, neuroactive ligand-receptor interaction, inflammatory response
Genetic and epigenetic methodologies have transformed HPA axis investigation, revealing complex regulatory networks underlying stress vulnerability and resilience. The field is progressing toward multi-omics frameworks that capture dynamic interactions across biological levels and timescales. Future methodologies will likely emphasize single-cell approaches, spatial omics in relevant brain regions, and time-resolved profiling during stress trajectories. These advances promise more precise understanding of HPA axis regulation and novel therapeutic strategies for stress-related disorders.
Experimental models of chronic stress are indispensable tools for deciphering the pathophysiology of stress-related disorders and developing novel therapeutic interventions. These models, primarily utilizing rodents, aim to recapitulate the complex neuroendocrine, behavioral, and physiological alterations observed in humans, with a particular focus on the hypothalamic-pituitary-adrenal (HPA) axis. This review provides a critical examination of the most prominent chronic stress paradigms, including Chronic Unpredictable Stress (CUS) and Chronic Social Defeat (CSD), evaluating their translational validity, methodological protocols, and inherent limitations. By synthesizing current data on behavioral, endocrine, and neurobiological outcomes, and framing these within the context of HPA axis dysregulation, this analysis aims to guide researchers in selecting appropriate models and interpreting findings for enhanced translational impact in drug development.
Chronic stress represents a state of prolonged perceived threat that challenges an organism's regulatory capacity, engaging a complex multisystem response fundamentally distinct from acute stress reactions [48]. The HPA axis serves as the primary neuroendocrine mediator of this response. In an acute stress situation, the hypothalamus releases corticotropin-releasing hormone (CRH), which stimulates the pituitary gland to secrete adrenocorticotropic hormone (ACTH), ultimately leading to the adrenal production of glucocorticoids (cortisol in humans, corticosterone in rodents) [7]. These glucocorticoids mobilize energy and modulate immune and neuronal function, while simultaneously activating negative feedback mechanisms to restore homeostasis.
Under chronic stress conditions, this finely tuned system becomes dysregulated. Persistent HPA axis activation can lead to impaired negative feedback, glucocorticoid receptor resistance, and paradoxical cortisol dysregulation, fostering a pro-inflammatory state and disrupting systemic homeostasis [7]. This maladaptive shift is implicated in the pathogenesis of numerous psychiatric, neurodegenerative, immune, and metabolic disorders [49] [15]. Therefore, experimental models that reliably recapitulate this transition from adaptive response to pathological state are crucial for biomedical research.
Prominent Rodent Models of Chronic Stress: Paradigms and Protocols
Chronic Unpredictable Stress (CUS) / Chronic Variable Stress (CVS)
The CUS paradigm is based on the principle that the unpredictability and uncontrollability of stressors prevent habituation and induce a state of sustained apprehension, more effectively modeling human depressive-like states than single or repeated homotypic stressors [48].
Detailed Experimental Protocol:
- Subjects: Typically, adult male rats or mice. Considerations of sex and age are critical, as these are determinants of stress response dynamics [50].
- Duration: 4 to 8 weeks.
- Stressors: Animals are exposed to one or two different stressors per day, administered in an unpredictable sequence. Common stressors include:
- Physical Restraint: Confinement in a well-ventilated tube for 1-2 hours.
- Forced Swim: In a water tank at room temperature for 5-15 minutes [51] [52].
- Social Isolation: Housing in individual cages for 24-48 hours [52].
- Cage Tilt: 45-degree cage tilt for several hours.
- Soiled Cage: Exposure to damp bedding for several hours.
- Light/Dark Cycle Alterations: Reversal of the light cycle or exposure to light during the dark phase [51].
- Food and Water Deprivation: Temporary removal for up to 24 hours.
Chronic Social Defeat (CSD)
The CSD model leverages the ethological relevance of social stress to induce robust, individual-specific phenotypes of susceptibility and resilience [48] [49].
Detailed Experimental Protocol:
- Subjects: Adult male mice, often using aggressive resident strains (e.g., CD1).
- Duration: 10 consecutive days.
- Procedure:
- Physical Defeat: An experimental C57BL/6 mouse is introduced into the home cage of an aggressive resident for 5-10 minutes, leading to physical subordination.
- Sensory Contact: Following the physical interaction, the experimental mouse is housed in a compartment within the resident's cage, separated by a perforated transparent divider, allowing continuous sensory contact for the remaining 24 hours.
- Rotation: The experimental mouse is exposed to a new, unfamiliar aggressor each day to prevent habituation.
- Phenotyping: After the stress period, mice are classified as "susceptible" or "resilient" based on their social interaction ratio in a novel environment with a target aggressor.
Table 1: Key Chronic Stress Models and Their Primary Characteristics
| Model | Core Principle | Duration | Key Stressors | Primary Outcome Measures |
|---|---|---|---|---|
| Chronic Unpredictable Stress (CUS) | Unpredictable, varied mild stressors preventing habituation | 4-8 weeks | Restraint, swim, isolation, light disruption [51] [52] | Anhedonia, anxiety-like behavior, HPA axis dysregulation [48] |
| Chronic Social Defeat (CSD) | Ethological stress from social subordination | 10 days | Physical defeat, continuous sensory contact [48] | Social avoidance, anhedonia, susceptible/resilient phenotypes [49] [48] |
| Social Isolation | Removal from social contact, mimicking a core human stressor | 4+ weeks | Single-housing in standard cages [52] | Anxiety-like behavior, aggression, altered neurochemistry [52] |
Quantitative Outcomes and Translational Validity
The utility of these models is gauged by their ability to produce measurable changes that mirror aspects of human pathology. The following table synthesizes common quantitative outcomes.
Table 2: Quantitative Behavioral and Physiological Outcomes in Chronic Stress Models
| Measured Parameter | Experimental Test | Change in Chronic Stress (vs. Control) | Translational Correlation |
|---|---|---|---|
| Anhedonia | Sucrose Preference Test | ↓ Preference for sweet solution [48] | Core symptom of Major Depressive Disorder (MDD) [15] |
| Anxiety-like Behavior | Open Field Test (OFT) | ↓ Time in center zone; ↑ thigmotaxis [51] | Anxiety disorders, often comorbid with MDD |
| Behavioral Despair | Forced Swim Test (FST) | ↑ Immobility time [52] | Passive coping strategy, related to hopelessness |
| Social Interaction | Social Interaction Test | ↓ Interaction time (in susceptible mice) [48] | Social withdrawal in depression and PTSD |
| HPA Axis Activity | Plasma Corticosterone | ↑ Basal levels; ↑ response to novel stressor [52] [48] | HPA axis hyperactivity in a subset of MDD patients [15] |
| Metabolic Change | Body Mass | ↓ Weight gain or weight loss [51] [48] | Appetite and weight changes in stress-related disorders |
Evaluating Validity
- Face Validity: CUS and CSD successfully produce behavioral changes (anhedonia, social withdrawal, anxiety) that resemble human depressive symptoms [49] [52].
- Construct Validity: These models are based on the etiological link between chronic stress exposure and the development of psychopathology. The dysregulation of the HPA axis and monoaminergic systems provides a sound neurobiological construct [49] [15].
- Predictive Validity: A key strength of models like CUS and CSD is their responsiveness to chronic, but not always acute, administration of standard antidepressant medications, accurately predicting clinical efficacy [48].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Chronic Stress Studies
| Item / Reagent | Function / Application | Example Use in Protocol |
|---|---|---|
| Restraint Apparatus | To induce psychological and physical stress. | Transparent or well-ventilated tubes for rodent restraint [50]. |
| Forced Swim Tank | To assess behavioral despair and/or as a stressor. | Cylindrical tank (e.g., 25°C water) for 5-15 min exposure [51]. |
| Sucrose Solution (1-2%) | To measure anhedonia via consumption preference. | Offered vs. water in a two-bottle choice test post-stress [48]. |
| Open Field Arena | To assess general locomotor activity and anxiety-like behavior. | A square arena; tracking time in center vs. periphery zones [51]. |
| Corticosterone ELISA Kit | To quantify HPA axis activity via plasma/serum corticosterone. | Measuring basal AM levels or stress-induced response [52]. |
| Antidepressants (e.g., Fluoxetine) | To validate model's predictive validity for drug screening. | Administered chronically via drinking water or injection [52] [48]. |
Neurobiological Underpinnings and HPA Axis Interactions
Chronic stress paradigms induce a cascade of neurobiological changes, with HPA axis dysregulation being a central component. The following diagram illustrates the core pathways involved in the chronic stress response and its impact on the HPA axis.
The HPA axis interacts bidirectionally with other key systems. The gut-brain axis (GBA) is a critical mediator, where stress-induced dysbiosis can increase intestinal permeability, allowing endotoxins like LPS to enter circulation and promote systemic and neuroinflammation, further exacerbating HPA axis dysfunction [15]. Furthermore, chronic stress leads to oxidative stress in brain regions such as the prefrontal cortex and hippocampus, and disrupts the production of neurotrophic factors like BDNF, which are crucial for neuronal health and plasticity [52].
Limitations and Future Directions
Despite their utility, chronic stress models possess significant limitations that must be considered when interpreting data.
- Adaptation vs. Pathology: A critical perspective is that many observed changes following chronic stress may represent adaptive survival strategies (e.g., metabolic shifts, risk aversion) rather than pure pathology. The transition to pathology may occur only when the organism's adaptive capacity is exhausted [48].
- Translational Gaps: The subjective emotional experience of stress in humans is impossible to fully replicate in rodents. Models relying on physical stressors may not adequately capture the complexity of psychological stress in humans [49].
- Individual Variability: Not all humans, or rodents, develop pathology after stress exposure. While the identification of "resilient" and "susceptible" phenotypes in models like CSD is a strength, the underlying mechanisms, particularly in metabolic regulation systems, are not fully understood [48] [49].
- Standardization Issues: Lack of standardization in the type, intensity, and duration of stressors across laboratories (e.g., variations in CUS protocols) can lead to inconsistent results, complicating direct comparisons [50].
Future research should focus on multi-omics approaches to identify novel biomarkers, develop models with improved psychological validity, and integrate data across biological levels to better understand the transition from resilience to pathology [49] [7]. The following diagram outlines a proposed workflow for utilizing these models in preclinical research, acknowledging their limitations.
Experimental models of chronic stress, particularly CUS and CSD, provide powerful, albeit imperfect, tools for investigating the neurobiology of stress-related disorders and screening potential therapeutics. Their strength lies in their ability to induce quantifiable behavioral and physiological changes rooted in HPA axis and neuroendocrine dysregulation, which show significant translational relevance. However, researchers must critically appraise findings within the context of each model's limitations, including the fine line between adaptation and pathology, and the inherent challenges in modeling human psychological stress in rodents. A nuanced approach that acknowledges these complexities, incorporates multidimensional phenotyping, and leverages emerging technologies will be essential for advancing our understanding of chronic stress and developing more effective treatments.
Bidirectional interactions between the neuroendocrine and immune systems represent a critical pathway through which psychological stress impacts health and disease. The hypothalamic-pituitary-adrenal (HPA) axis serves as the principal neuroendocrine mediator of stress responses, primarily through cortisol secretion, which influences immune regulation and systemic homeostasis [7]. Simultaneously, immune activation signals back to the CNS, shaping stress responsiveness and contributing to stress-related pathologies [17]. This intricate crosstalk has been implicated in numerous conditions, including major depressive disorder, bipolar disorder, autoimmune diseases, and neuroendocrine neoplasms [17] [7] [53].
Assessing this bidirectional communication requires specialized methodologies that can capture the dynamic, multi-system nature of these interactions. Two cornerstone approaches in contemporary stress research are the measurement of cytokine profiles to characterize immune status and glucocorticoid sensitivity testing to evaluate target tissue responsiveness to cortisol signals [54]. These assays provide crucial insights into how stress disrupts physiological balance and contributes to the development and progression of various disorders. This technical guide details the experimental protocols, analytical approaches, and practical implementation of these key assays for researchers and drug development professionals working in stress research and related fields.
Cytokine Profiling in Stress and Psychiatric Research
Cytokine profiling provides a quantitative assessment of immune system activity, particularly the inflammatory status, which is frequently altered in stress-related conditions.
Key Cytokine Alterations in Psychiatric and Stress Disorders
Meta-analyses have firmly established that individuals with major depressive disorder (MDD) show elevated levels of specific pro-inflammatory cytokines and acute-phase proteins compared to healthy controls [17]. The table below summarizes the most consistently documented cytokine alterations in MDD patients.
Table 1: Characteristic Cytokine Profile Alterations in Major Depressive Disorder (MDD)
| Cytokine / Marker | Direction of Change in MDD | Functional Role |
|---|---|---|
| IL-6 | ↑ | Pro-inflammatory cytokine; induces acute phase protein production |
| TNF-α | ↑ | Pro-inflammatory cytokine; regulates immune cell apoptosis & inflammation |
| sIL-2R | ↑ | Soluble receptor; marker of T-cell activation |
| IL-1RA | ↑ | Receptor antagonist; endogenous regulator of IL-1 activity |
| CRP | ↑ | Acute-phase protein; general marker of systemic inflammation |
| IL-10 | ↑ (Meta-analysis) | Anti-inflammatory cytokine; modulates pro-inflammatory responses |
| IFN-γ | ↓ (Meta-analysis) | Pro-inflammatory cytokine; primary activator of macrophages |
These inflammatory profiles are not specific to MDD but represent a potential shared immune pathway across psychiatric disorders, including bipolar disorder and schizophrenia, particularly during acute symptomatic phases [17]. The source of these cytokines includes not only peripheral immune cells but also activated glial cells within the central nervous system, contributing to neuroinflammation [53].
Experimental Protocol for Cytokine Measurement
Sample Collection and Preparation:
- Sample Type: Plasma or serum from peripheral blood. For stimulated cytokine production, diluted whole blood or isolated Peripheral Blood Mononuclear Cells (PBMCs) are used [54].
- Collection: Blood collected into anticoagulant tubes (e.g., heparin or EDTA). For serum, use serum separator tubes.
- Processing: Centrifuge blood samples to isolate plasma/serum. Aliquot and store at -80°C until analysis to prevent cytokine degradation.
Measurement Techniques:
- Enzyme-Linked Immunosorbent Assay (ELISA): A standard workhorse for quantifying specific cytokines in a single-plex format. It is widely accessible and cost-effective but has a limited dynamic range, often requiring sample dilution for accurate measurement in stimulated whole-blood assays [54].
- Multiplex Immunoassays (e.g., Luminex): This technology allows for the simultaneous quantification of multiple cytokines (e.g., IL-6, TNF-α, IL-1β, IL-10) from a single small-volume sample. This is highly efficient for generating broad cytokine profiles and is increasingly common in clinical and translational research [17] [54].
Stimulated vs. Unstimulated Measures:
- Basal Levels: Measuring circulating cytokines in plasma/serum provides a snapshot of the in vivo inflammatory state.
- Stimulated Production: Incubating whole blood or PBMCs with mitogens like Lipopolysaccharide (LPS) (activates innate immunity via monocytes) or Phytohemagglutinin (PHA) (activates T-cells) assesses the functional capacity of immune cells to produce cytokines upon challenge. This can reveal immune system priming that is not apparent from basal levels alone [54].
Glucocorticoid Sensitivity Testing
Glucocorticoid sensitivity refers to the responsiveness of target tissues to the anti-inflammatory and immunomodulatory signals of glucocorticoids. In chronic stress and related psychiatric conditions, a state of reduced sensitivity or glucocorticoid resistance can develop, leading to impaired containment of inflammatory responses [54].
In Vitro Whole Blood Assay for Glucocorticoid Sensitivity
The most frequently used and robust method for assessing glucocorticoid sensitivity of the immune system is the in vitro whole blood assay with lipopolysaccharide (LPS) stimulation [54].
Principle: The assay measures the ability of synthetic (dexamethasone, DEX) or natural (hydrocortisone, HC) glucocorticoids to suppress the production of pro-inflammatory cytokines (e.g., IL-6, TNF-α) from immune cells stimulated by LPS.
Protocol Workflow:
Diagram 1: Glucocorticoid Sensitivity Assay Workflow
Detailed Step-by-Step Protocol:
- Blood Collection & Preparation: Draw venous blood into heparinized tubes (other anticoagulants like citrate can be toxic to cells). Dilute the whole blood with saline at a standard ratio (e.g., 1:10) [54].
- Experimental Setup: Aliquot the diluted blood into sterile cell culture plates. Add:
- LPS: A standardized concentration (e.g., 1-10 ng/mL) to activate innate immune cells and trigger cytokine production.
- Dexamethasone (DEX): A range of concentrations (typically from 10⁻⁹ M to 10⁻⁶ M) to generate a dose-response curve. Include a control well with LPS but no DEX to determine maximum cytokine production.
- Incubation: Incubate the plates for a standardized period (6-24 hours) at 37°C with 5% CO₂ [54].
- Sample Harvest: Centrifuge the plates to pellet cells and collect the supernatant for cytokine analysis.
- Cytokine Measurement: Quantify the concentration of a target cytokine (e.g., IL-6) in the supernatant using ELISA or multiplex assays. The high cytokine concentrations in supernatants often require pre-dilution before analysis [54].
Data Analysis and Interpretation:
- IC₅₀ Calculation: For each participant, a dose-response curve is fitted using non-linear regression. The half-maximal inhibitory concentration (IC₅₀) is calculated, representing the concentration of DEX required to suppress 50% of the LPS-induced cytokine production.
- Interpretation: A higher IC₅₀ value indicates lower glucocorticoid sensitivity (i.e., more DEX is needed to suppress the immune response), a state often referred to as glucocorticoid resistance. A lower IC₅₀ indicates higher sensitivity [54].
Clinical Relevance and Research Findings
This assay has revealed that reduced glucocorticoid sensitivity is associated with chronic stress conditions, such as caregiving, vital exhaustion, and Major Depressive Disorder (MDD) [54]. In contrast, conditions like Post-Traumatic Stress Disorder (PTSD) are often associated with increased glucocorticoid sensitivity [54]. These alterations are clinically relevant, as reduced sensitivity predicts higher plasma inflammation and increased susceptibility to infections like the common cold [54].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of these assays requires specific, high-quality reagents. The table below lists the essential components.
Table 2: Key Research Reagents for Neuroendocrine-Immune Assays
| Reagent / Material | Function / Purpose | Example & Notes |
|---|---|---|
| Heparinized Blood Tubes | Anticoagulant for whole blood collection | Preferred over citrate or EDTA for cell culture viability. |
| Lipopolysaccharide (LPS) | Toll-like receptor 4 agonist; stimulates innate immune cells & cytokine production | E. coli LPS; batch-to-batch variability requires pre-testing. |
| Phytohemagglutinin (PHA) | T-cell mitogen; stimulates T-cell proliferation & cytokine production | Used for assessing GC sensitivity in cellular immunity. |
| Dexamethasone (DEX) | Synthetic glucocorticoid; used for in vitro dose-response curves | High affinity for GR; displaces endogenous cortisol in assay. |
| Hydrocortisone (HC) | Natural glucocorticoid (cortisol); alternative to DEX | More physiologically analogous but lower affinity than DEX. |
| Cell Culture Plates & CO₂ Incubator | Provide sterile environment for ex vivo cell incubation | Standard 37°C, 5% CO₂ incubation. |
| Cytokine Detection Kit | Quantify cytokine concentrations in supernatants/plasma | ELISA kits or Multiplex panels (e.g., for IL-6, TNF-α, IL-10). |
Integrated Signaling Pathways in Neuroendocrine-Immune Communication
The assays described above measure the functional output of complex, bidirectional biological pathways. The following diagram integrates the core signaling mechanisms linking the HPA axis and the immune system, highlighting points measured by these assays.
Diagram 2: Integrated HPA-Immune Signaling & Assay Measurement
The diagram illustrates key interactions: 1) GC Signaling: Cortisol binds to cytosolic Glucocorticoid Receptors (GR) in immune cells, leading to transrepression of pro-inflammatory genes (e.g., for IL-6, TNF-α). 2) Intracellular Signaling: Stressors and cytokines can activate pro-inflammatory pathways like NF-κB and MAPK in immune cells. 3) Immune to HPA Axis Feedback: Pro-inflammatory cytokines can activate the HPA axis at multiple levels, increasing cortisol production. 4) Assay Measurement: The in vitro GC sensitivity assay (point 4) directly tests the functional integrity of the pathway outlined in point 1 by applying DEX and measuring cytokine suppression.
The hypothalamic-pituitary-adrenal (HPA) axis serves as the body's primary neuroendocrine stress response system, coordinating adaptive physiological reactions to psychological and physical stressors. Dysregulation of this axis represents a fundamental pathophysiological mechanism in stress-related disorders, including major depressive disorder (MDD) and alcohol use disorder (AUD) [7] [55]. Upon stress exposure, corticotropin-releasing hormone (CRH) is synthesized in the paraventricular nucleus (CRH) of the hypothalamus and stimulates anterior pituitary secretion of adrenocorticotropic hormone (ACTH), which subsequently prompts glucocorticoid release (cortisol in humans, corticosterone in rodents) from the adrenal cortex [56] [17]. This cascade ultimately elevates circulating glucocorticoid levels, which through negative feedback mechanisms at hippocampal, hypothalamic, and pituitary glucocorticoid receptors (GRs), normally suppress further CRH and ACTH release [55] [57].
In chronic stress states, this meticulously regulated system becomes profoundly dysregulated. Persistent HPA axis activation leads to impaired GR-mediated negative feedback, glucocorticoid receptor resistance, and paradoxical cortisol dysregulation [7] [55]. The resulting hypercortisolemia exerts neurotoxic effects, particularly within the hippocampus and prefrontal cortex (PFC), contributing to neuronal atrophy, synaptic plasticity deficits, and reduced neurogenesis [58] [17]. Concurrently, chronic stress promotes a pro-inflammatory state characterized by elevated pro-inflammatory cytokines, including interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), which further perpetuates neuroendocrine and neuroimmune dysfunction [55] [17]. This complex pathophysiology has prompted targeted drug discovery efforts aimed at specific components of the HPA axis and associated signaling pathways, with CRH antagonists and selective glucocorticoid receptor modulators representing two prominent therapeutic approaches.
Corticotropin-Releasing Hormone (CRH) Antagonists
CRH Type 1 Receptor (CRHR1) as a Therapeutic Target
CRH, a 41-amino acid neuropeptide, initiates the HPA axis stress response through binding to CRH type 1 receptors (CRHR1), G-protein coupled receptors (GPCRs) widely distributed throughout the central nervous system (CNS) [56]. CRHR1 activation triggers multiple intracellular signaling pathways, including mitogen-activated protein kinase (MAPK), protein kinase A (PKA), and phospholipase C (PLC) pathways, which modulate synaptic plasticity, neuroinflammatory responses, and autophagy-related processes [56]. Extensive preclinical evidence points to a central role of CRHR1 in mediating stress-induced depressive phenotypes, with CRHR1 upregulation observed in key brain regions involved in mood regulation, including the amygdala [59] [56].
The amygdala, a hub for emotional processing, contains intercalating cell masses (ITC) highly enriched with both CRHR1 and dopamine D1 receptors, suggesting functional interaction between stress and reward pathways [59]. Pharmacological activation of CRHR1 in the amygdala/ITC increases anxiety-like behavior in the Elevated-Plus-Maze test, an effect prevented by co-administration of the D1 antagonist SCH23390 [59]. Furthermore, alcohol-dependent rats show upregulated amygdala CRHR1 expression linked to increased behavioral sensitivity to stress, alcohol intake, and seeking behavior [59]. Despite robust preclinical evidence supporting CRHR1 blockade for reducing anxiety, alcohol consumption, and relapse behavior, clinical trials with CRHR1 antagonists in AUD and other psychiatric conditions have largely failed, highlighting the complexity of CRH system pathophysiology and challenges in clinical translation [59] [56].
Experimental Models and Methodologies for CRHR1 Research
Table 1: Key Research Reagents for CRHR1 Investigations
| Reagent / Model | Specific Example | Research Application / Function |
|---|---|---|
| CRHR1 Agonists | CRH (2 μg/μL), Stressin I (4 μg/2 μL) | Pharmacological activation of CRHR1; demonstrates increased D1 binding in amygdala [59] |
| CRHR1 Antagonists | (Multiple compounds in development) | Block CRHR1 signaling to assess behavioral and neurobiological correlates [56] |
| D1 Receptor Antagonist | SCH23390 (120 ng/0.5 μL) | Blocks dopamine D1 receptors; prevents CRHR1-mediated anxiogenic effects in ITC [59] |
| Genetic Models | D1Cre-Crhr1−/− knockout mice | Determines cell-type specific CRHR1 functions and interactions with dopamine signaling [59] |
| Rodent Behavioral Assays | Elevated-Plus-Maze (EPM), Two-Bottle-Free-Choice, Forced Swim Stress-induced drinking | Measures anxiety-like behavior, alcohol consumption, and stress-induced drinking [59] |
| Neuroanatomical Techniques | D1 receptor autoradiography, in situ hybridization, Golgi-impregnation, Crhr1-GFP reporter mice | Quantifies receptor binding, gene expression, neuronal morphology, and receptor localization [59] |
| Immunohistochemistry | Double-immunofluorescence for D1 and CRHR1 | Visualizes receptor co-localization and interaction in specific brain regions [59] |
Detailed Experimental Protocol: Assessing CRHR1-D1 Receptor Interactions in the Amygdala
- Animal Subjects: Adult male and female rats (e.g., Sprague-Dawley) or genetically modified mice (e.g., D1Cre-Crhr1−/−, Crhr1-GFP reporter mice).
- Surgical Procedures: Anesthetize animals and implant guide cannulae stereotaxically targeting the intracerebroventricular (i.c.v.) space or specific amygdala nuclei (e.g., ITC), using standard aseptic techniques.
- Drug Administration:
- Behavioral Testing: Subject animals to the Elevated-Plus-Maze (EPM) 10-15 minutes post-injection to quantify anxiety-like behavior (time spent in open arms, entries into open vs. closed arms) [59].
- Tissue Collection and Analysis:
- Euthanize animals and rapidly extract brains.
- For receptor autoradiography: Process fresh-frozen brain sections using saturating concentrations of radioactive ligands (e.g., [³H]SCH23390) to quantify D1 receptor binding sites, particularly in the amygdala [59].
- For immunohistochemistry: Perfuse-fix brains, section, and incubate with primary antibodies against D1 and CRHR1, followed by species-appropriate fluorescent secondary antibodies to visualize co-localization [59].
- For in situ hybridization: Process sections with riboprobes targeting D1 receptor mRNA to assess transcriptional regulation [59].
- Data Analysis: Employ appropriate statistical methods (e.g., ANOVA with post-hoc tests) to compare behavioral scores and neurobiological markers between experimental groups.
Figure 1: CRHR1 Signaling in Amygdala and Stress-Related Behaviors. This diagram illustrates the stress-induced CRH release and subsequent CRHR1 activation in amygdala circuits, particularly highlighting the interaction with dopamine D1 receptors in ITC neurons that leads to disinhibition of the central amygdala (CeA) and promotes anxiety and alcohol-seeking behaviors. The point of pharmacological intervention by CRHR1 antagonists is also shown.
Selective Glucocorticoid Receptor Modulators (SEGRAMs)
Dissociating Transrepression from Transactivation
Glucocorticoids are highly effective anti-inflammatory agents but their long-term clinical utility is severely limited by metabolic adverse effects including hyperglycemia, diabetes, and osteoporosis [60]. These undesirable effects are primarily mediated via GR transactivation (direct DNA binding and regulation of gene transcription), whereas the anti-inflammatory effects largely result from transrepression (protein-protein interactions with transcription factors like NF-κB) [60]. Selective glucocorticoid receptor agonists and modulators (SEGRAMs) represent a novel class of non-steroidal compounds designed to exploit this mechanistic dichotomy, retaining therapeutic transrepression efficacy while minimizing adverse transactivation effects [60].
GRM-01 is a novel, orally available, non-steroidal SEGRAM currently in Phase 1 clinical development. In vitro binding assays demonstrate that GRM-01 is a potent and selective ligand of human GR versus human progesterone and mineralocorticoid receptors (inhibition constant Ki = 12 vs. 3,700 and >10,000 nM, respectively) [60]. GRM-01 displays partial induction at the GR (transactivation EC₅₀ = 60.2 nM, efficacy 31.8%) compared to prednisolone (EC₅₀ = 24.3 nM, efficacy 80.5%), indicating its dissociated profile [60]. Crucially, GRM-01 demonstrates potent anti-inflammatory efficacy in functional assays, inhibiting TNF-α and IFN-γ release in whole blood and IL-6 release in cellular assays, while only weakly inducing markers of glucose metabolism (tyrosine aminotransferase activity) and bone metabolism (osteoprotegerin release) compared to conventional glucocorticoids [60].
Quantitative Profiling of SEGRAM Activity
Table 2: Preclinical Pharmacological Profile of GRM-01 Versus Prednisolone
| Pharmacological Parameter | GRM-01 | Prednisolone | Experimental Context / Significance |
|---|---|---|---|
| GR Binding (Ki, nM) | 12 | Not reported | Human GR in IM-9 cell lysates; indicates high target affinity [60] |
| GR Transactivation (EC₅₀, nM) | 60.2 | 24.3 | Reporter gene assay; partial efficacy (31.8% vs 80.5%) suggests dissociated profile [60] |
| Anti-inflammatory Efficacy | Inhibits TNF-α, IFN-γ, IL-6 | Inhibits cytokines | Functional assays in human whole blood and lung cells; demonstrates maintained transrepression [60] |
| TAT Induction (% efficacy) | 14.0 | 92.4 | In HepG2 cells; marker of gluconeogenic effect; reduced potential for hyperglycemia [60] |
| OPG Inhibition (% max) | 58 | 100 | In MG-63 osteoblasts; marker of bone adverse effects; reduced risk of osteoporosis [60] |
| In vivo Anti-inflammatory | Reduces ankle swelling | Reduces swelling | Rat model of inflammation; confirms in vivo efficacy [60] |
| In vivo Blood Glucose | No increase | Increases glucose | Differentiates from classic glucocorticoid metabolic effects [60] |
| Predicted Human t₁/₂ (h) | ~98 | ~3.5 | Based on animal PK; suggests once-daily or less frequent dosing potential [60] |
Detailed Experimental Protocol: Characterizing SEGRAM Activity In Vitro
- Nuclear Hormone Receptor Binding Assays:
- GR Binding: Incubate lysates from human B lymphoblast IM-9 cells (which endogenously express GR) with GRM-01 or reference compound (e.g., prednisolone) and the radioligand ³H-dexamethasone (1.5 nM final concentration) for 6 hours at 4°C. Determine half-maximal inhibitory concentration (IC₅₀) and inhibition constant (Ki) via scintillation counting and nonlinear regression analysis [60].
- Selectivity Screening: Similarly, test binding affinity for human progesterone receptor (PR) in T47D breast carcinoma cells using ³H-progesterone (0.5 nM), and for mineralocorticoid receptor (MR) in Sf9 cells recombinantly overexpressing human MR using ³H-aldosterone (0.4 nM) [60].
- GR Transactivation Reporter Gene Assay:
- Culture cells (e.g., U2OS human osteosarcoma) stably transfected with a GR-responsive reporter gene (e.g., MMTV-luciferase).
- Treat cells with serial dilutions of GRM-01, prednisolone, or vehicle for a standardized period (e.g., 24 hours).
- Measure luciferase activity as a marker of GR-mediated gene transcription. Calculate EC₅₀ and efficacy relative to a full agonist [60].
- Functional Anti-inflammatory Assays:
- Whole Blood Assay: Incubate fresh human or rat blood with lipopolysaccharide (LPS) to induce inflammatory cytokine release (TNF-α, IFN-γ) in the presence or absence of test compounds. Quantify cytokine levels in supernatant via ELISA [60].
- Cellular Assays: Use human lung cells or primary fibroblast-like synoviocytes from rheumatoid arthritis patients. Stimulate with appropriate agonists (e.g., IL-1β) and measure inhibition of IL-6 release by test compounds via ELISA [60].
- Adverse Effect Marker Assays:
- Tyrosine Aminotransferase (TAT) Induction: Treat human hepatoma HepG2 cells with test compounds for 24-48 hours. Measure TAT enzyme activity spectrophotometrically as a marker of gluconeogenesis and hyperglycemia risk [60].
- Osteoprotegerin (OPG) Inhibition: Treat human osteosarcoma MG-63 cells with test compounds. Quantify OPG release into supernatant via ELISA as a marker of bone metabolism disruption [60].
Figure 2: SEGRAM Mechanism: Dissociated GR Modulation. This diagram illustrates the mechanism of action of Selective Glucocorticoid Receptor Agonists and Modulators (SEGRAMs). SEGRAMs bind the GR and induce a conformational change that favors transrepression (therapeutic anti-inflammatory effects) over transactivation (linked to adverse metabolic effects), thereby potentially improving the therapeutic window.
Emerging and Novel Therapeutic Targets
Beyond direct HPA axis components, recent research has identified several promising novel targets within the broader neuroendocrine-immune network that contribute to stress pathophysiology.
Gut-Brain Axis and Microbial Therapeutics: Chronic stress disrupts the gut microbiota composition (dysbiosis), increasing intestinal permeability and allowing bacterial endotoxins (e.g., LPS) to enter circulation, triggering systemic and neuroinflammation [15]. This inflammatory state can impair HPA axis feedback sensitivity. Therapeutic strategies include prebiotics, probiotics, and postbiotics to restore healthy gut microbiota, potentially reducing inflammation and ameliorating depressive symptoms [15].
Kynurenine Pathway Metabolites: Under chronic stress and inflammation, the metabolism of the essential amino acid tryptophan shifts away from serotonin production toward the kynurenine pathway [55]. This leads to increased production of neurotoxic metabolites such as quinolinic acid (an NMDA receptor agonist), which can contribute to neurotoxicity, hippocampal atrophy, and impaired neuroplasticity in TRD [55]. Inhibiting key enzymes in this pathway (e.g., IDO, KMO) represents a novel strategy to rebalance tryptophan metabolism.
Synaptic Plasticity and Rapid-Acting Antidepressants: Chronic stress and glucocorticoid excess reduce brain-derived neurotrophic factor (BDNF) levels and promote synaptic deficits in prefrontal and limbic regions [58]. The rapid antidepressant effects of ketamine are believed to act, in part, by rapidly restoring synaptic connectivity and reversing stress-induced neuronal atrophy via mechanisms that involve increased BDNF release and activation of mTOR signaling, highlighting synaptic plasticity as a critical therapeutic target [55].
The continued investigation of CRH antagonists, SEGRAMs, and novel targets within the extended neuroendocrine-immune network represents a promising frontier for developing more effective and better-tolerated therapeutics for stress-related disorders. The future of this field lies in embracing the complexity of these systems, including their intricate bidirectional communication (e.g., gut-brain axis) and the role of epigenetic modifications that may underlie treatment resistance [55]. A successful therapeutic strategy will likely require a multi-target approach, potentially combining HPA axis modulation with interventions that address inflammation, oxidative stress, and synaptic plasticity. Furthermore, personalizing treatments based on individual HPA axis phenotype, genetic makeup, and inflammatory biomarker profiles may be key to improving clinical outcomes for complex conditions like major depressive disorder and alcohol use disorder.
The hypothalamic-pituitary-adrenal (HPA) axis represents the body's primary neuroendocrine stress response system, integrating neural and hormonal signals to maintain homeostasis under challenging conditions [61] [62]. This sophisticated pathway begins with corticotropin-releasing hormone (CRH) release from the paraventricular nucleus (PVN) of the hypothalamus, which stimulates anterior pituitary secretion of adrenocorticotropic hormone (ACTH), ultimately driving cortisol production from the adrenal cortex [61]. Under healthy conditions, this system operates with precise negative feedback control, where circulating cortisol suppresses further CRH and ACTH release, restoring physiological equilibrium once the stressor subsides [61]. The HPA axis follows a circadian rhythm characterized by pulsatile cortisol secretion that peaks approximately 30-45 minutes after waking and gradually declines throughout the day [61].
When stress becomes chronic, the finely tuned HPA axis can become dysregulated through several established mechanisms. Glucocorticoid receptor resistance develops, diminishing cortisol's ability to suppress inflammatory responses [7] [61]. The negative feedback system becomes impaired, leading to sustained cortisol secretion even in the absence of immediate threats [61]. Over time, this may progress to adrenal exhaustion, characterized by reduced adrenal cortex responsiveness to ACTH and a paradoxical state of hypocortisolism despite persistent stress [61]. This dysregulation creates a pro-inflammatory state with elevated pro-inflammatory cytokines (IL-1β, IL-6, TNF-α) and reduced anti-inflammatory signaling, establishing a pathological link between chronic stress and various disease states [61].
Stress Resilience Pathways and Mechanisms
Stress resilience represents the adaptive capacity to maintain physiological and psychological homeostasis despite significant adversity. Several key neural pathways and molecular mechanisms underlie this resilience:
The prefrontal cortex-amygdala circuit plays a critical role in top-down regulation of stress responses. Resilience is associated with effective prefrontal inhibition of amygdala hyperactivity, while impaired regulation leads to exaggerated fear and stress responses [62]. Neuroimaging studies reveal that resilient individuals display enhanced connectivity between regulatory prefrontal regions and limbic emotion-processing centers [62].
At the molecular level, glucocorticoid receptor sensitivity significantly influences resilience. Maintained receptor sensitivity ensures appropriate feedback inhibition of the HPA axis, while receptor resistance leads to prolonged activation and inadequate containment of inflammatory processes [7] [61]. The endocannabinoid system also contributes to resilience through its modulatory effects on both HPA axis activity and emotional processing, with evidence suggesting it mediates some stress-buffering effects of physical activity [63].
Neuroplasticity mechanisms, including hippocampal neurogenesis and dendritic remodeling in prefrontal circuits, represent additional resilience factors. Chronic stress typically reduces synaptic plasticity and promotes neuronal atrophy in these regions, whereas interventions that enhance brain-derived neurotrophic factor (BDNF) signaling can counteract these detrimental effects [64] [63].
Non-Pharmacological Intervention Modalities
Mind-Body and Psychological Interventions
Table 1: Mind-Body and Psychological Interventions for HPA Axis Modulation
| Intervention Category | Specific Techniques | Physiological Mechanisms | Measured Outcomes |
|---|---|---|---|
| Mindfulness & Mind-Body Practices | Mindfulness-Based Stress Reduction (MBSR), Yoga, Tai Chi, Meditation | Reduced cortisol awakening response, Enhanced heart rate variability, Increased prefrontal cortex activity | Decreased perceived stress, Reduced anxiety scores, Improved heart rate variability |
| Psychological Adaptation Training | Cognitive Behavioral Therapy (CBT), Emotion Regulation Training, Breathing Exercises | Normalization of diurnal cortisol rhythm, Improved glucocorticoid receptor sensitivity, Reduced amygdala reactivity | Lower depression inventory scores, Reduced burnout scales, Improved emotion regulation capacity |
| Digital Cognitive-Behavioral Interventions | Internet-based CBT, Mobile health apps, Virtual reality exposure therapy | Modification of cognitive-affective networks, Attenuated sympathetic nervous system response | Decreased psychological distress scores, Improved stress coping measures, Enhanced treatment accessibility |
Mind-body interventions demonstrate significant efficacy for HPA axis regulation. Mindfulness-based practices produce measurable reductions in cortisol output and inflammatory markers while improving heart rate variability, indicating enhanced autonomic regulation [65] [66]. These practices are associated with structural brain changes in regions involved in emotional regulation, including increased prefrontal cortex thickness and reduced amygdala volume [64].
Cognitive-behavioral approaches target maladaptive thought patterns that perpetuate stress responses while building cognitive flexibility. Studies document normalization of diurnal cortisol patterns following CBT interventions, with particular benefits for populations facing chronic stress such as healthcare workers and disaster responders [65]. Emotion regulation training enhances prefrontal inhibition of limbic reactivity, potentially reversing the neurobiological effects of chronic stress [65] [62].
Digital interventions represent an emerging modality with particular utility for accessibility and scalability. Internet-based cognitive behavioral therapy demonstrates significant effects on stress symptomatology, while virtual reality applications show promise for exposure-based therapies and stress inoculation training [65].
Physical Activity and Exercise Interventions
Table 2: Exercise Modalities and HPA Axis Regulation
| Exercise Modality | Protocol Parameters | HPA Axis Effects | Resilience Outcomes |
|---|---|---|---|
| Moderate Aerobic Exercise | 30-45 minutes, 3-5 days/week, 60-75% HRmax | Blunted cortisol response to psychosocial stress, Enhanced cortisol recovery, Increased insulin sensitivity | Improved stress reactivity, Reduced depressive symptoms, Enhanced cardiovascular fitness |
| Resistance Training | 2-3 days/week, 8-10 exercises, 2-4 sets, 8-12 reps | Transient acute cortisol increases without chronic elevation, Improved anabolic balance | Reduced anxiety measures, Increased muscle mass, Improved metabolic parameters |
| Mind-Body Exercise | Yoga, Tai Chi: 2-3 sessions/week, 45-60 minutes | Reduced basal cortisol levels, Decreased inflammatory markers, Increased GABAergic activity | Enhanced perceived stress scores, Improved sleep quality, Better balance and flexibility |
Physical activity represents a powerful non-pharmacological approach to HPA axis regulation. Aerobic exercise at moderate intensity produces a trained response characterized by more rapid cortisol recovery following psychosocial stress exposure [63]. Regular aerobic activity is associated with reduced inflammatory signaling and increased anti-inflammatory mediators, countering the pro-inflammatory state of chronic stress [63].
Resistance training demonstrates particular benefits for psychological resilience, with meta-analyses confirming reductions in anxiety symptoms across diverse populations [63]. The transient cortisol increases during acute resistance sessions appear to represent an adaptive hormonal response rather than a maladaptive stress pattern, ultimately contributing to metabolic resilience through improved body composition and glucose regulation [63].
Mind-body exercises such as yoga and tai chi uniquely integrate physical movement with breath awareness and meditative components. These practices are associated with increased parasympathetic tone and significant reductions in perceived stress scores, making them particularly suitable for individuals with limited exercise capacity or heightened stress reactivity [63].
Lifestyle and Circadian Interventions
Sleep-wake cycle regulation represents a foundational element of HPA axis health. The HPA axis and sleep systems maintain a bidirectional relationship, with cortisol rhythm influencing sleep architecture and sleep quality affecting HPA regulation [67]. Interventions targeting sleep hygiene—including consistent sleep-wake times, darkness exposure, and pre-sleep routines—demonstrate significant effects on cortisol patterns, particularly the cortisol awakening response [67].
Dietary approaches that support HPA axis function emphasize nutrient density and meal timing. Key nutritional elements include B vitamins (cofactors in catecholamine synthesis), magnesium (modulation of NMDA receptor activity and HPA responsiveness), and omega-3 fatty acids (anti-inflammatory and neuroprotective effects) [67]. Evidence supports the strategic use of adaptogenic herbs—including ashwagandha, rhodiola, and holy basil—which appear to modulate stress system activity without direct stimulation or inhibition [68] [67].
Social connectivity and community engagement influence HPA function through neuropeptide pathways, particularly oxytocin, which demonstrates cortisol-buffering properties [66] [69]. Building diverse social networks and participating in meaningful group activities correlates with flatter diurnal cortisol slopes and reduced cortisol reactivity to laboratory stressors [66] [69].
Experimental Methodologies and Assessment Protocols
HPA Axis Function Testing Protocols
Salivary cortisol assessment provides a non-invasive method for evaluating HPA axis dynamics. The cortisol awakening response (CAR) protocol requires participants to collect saliva samples immediately upon waking, then at 30, 45, and 60 minutes post-awakening to capture the natural cortisol spike [68] [67]. For diurnal cortisol profiling, samples are typically collected at 4-6 timepoints throughout the day (e.g., 9:00, 12:00, 15:00, 18:00, 21:00) to establish the circadian rhythm [68].
The Dexamethasone Suppression Test (DST) evaluates HPA axis negative feedback integrity. Laboratory protocols typically administer 0.5-1.0 mg dexamethasone orally at 11:00 PM, with blood or saliva cortisol measurement the following morning between 8:00-9:00 AM [61]. In research settings, the Dexamethasone-CRH combined test provides enhanced sensitivity by administering CRH after dexamethasone pretreatment, with cortisol and ACTH measurements at 15-minute intervals for 90-120 minutes post-CRH [61].
For stress reactivity assessment, the Trier Social Stress Test (TSST) represents the gold standard laboratory stressor. The standardized protocol includes a 10-minute preparation period, followed by a 10-minute public speaking task and 10-minute mental arithmetic before a panel of evaluators, with cortisol and physiological measurements at baseline, immediately post-stress, and at 10, 20, 30, 45, 60, and 90 minutes recovery [61].
Psychophysiological Assessment Methods
Heart rate variability (HRV) measurement provides a non-invasive index of autonomic nervous system balance, with specific frequency domain parameters (particularly low frequency/high frequency ratio) reflecting sympathovagal balance. Standardized protocols require controlled breathing (typically 6 breaths/minute) and measurement durations of 5-15 minutes under resting conditions [63].
Psychometric assessment typically includes validated self-report measures such as the Perceived Stress Scale (PSS), Depression Anxiety Stress Scales (DASS), Connor-Davidson Resilience Scale (CD-RISC), and specific measures for burnout (Maslach Burnout Inventory) and post-traumatic stress (PCL-5) [65].
Intervention-Specific Methodologies
Mindfulness-based intervention protocols typically follow the 8-week Mindfulness-Based Stress Reduction (MBSR) structure developed by Kabat-Zinn, including weekly 2.5-hour group sessions, one full-day retreat, and daily 45-minute home practice [65]. Exercise intervention studies commonly employ supervised laboratory-based sessions 3-5 times weekly for 8-16 weeks, with precise intensity monitoring via heart rate or VO₂ measurement [63]. Cognitive-behavioral therapy protocols for stress typically encompass 12-16 weekly sessions incorporating cognitive restructuring, behavioral activation, and stress inoculation techniques [65].
Research Reagent Solutions and Methodological Tools
Table 3: Essential Research Reagents for HPA Axis and Stress Resilience Studies
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Immunoassay Kits | Salivary cortisol ELISA, Salivary cortisone LC-MS/MS, Inflammatory cytokine panels | HPA axis activity profiling, Circadian rhythm assessment, Inflammation monitoring | Sample stability requirements, Cross-reactivity profiles, Sensitivity to interfering substances |
| Molecular Biology Reagents | Glucocorticoid receptor antibodies, CRH mRNA probes, DNA methylation kits for NR3C1 | Receptor expression quantification, Epigenetic regulation studies, Gene expression profiling | Tissue fixation methods, Antibody specificity validation, Bisulfite conversion efficiency |
| Neuroimaging Tracers | [¹¹C]carfentanil (μ-opioid), [¹¹C]WAY-100635 (5-HT₁A), [¹⁸F]FDG (glucose metabolism) | Neurotransmitter system dynamics, Brain metabolic activity, Receptor availability | Radiotracer half-life, Receptor binding specificity, Quantification methods |
Additional essential research tools include laboratory stress induction systems such as the Trier Social Stress Test (TSST) standardized equipment and protocols [61]. Ambulatory monitoring devices for heart rate variability, actigraphy, and ecological momentary assessment enable real-world data collection in natural environments [63]. Genetic and epigenetic analysis platforms facilitate examination of stress-related gene polymorphisms (e.g., FKBP5, NR3C1) and DNA methylation patterns in candidate genes [7] [61].
Pathway Diagrams and Conceptual Frameworks
Non-pharmacological approaches to HPA axis modulation represent promising avenues for enhancing stress resilience through multiple neurobiological mechanisms. The evidence supports targeted lifestyle interventions—including physical activity, mindfulness practices, cognitive-behavioral strategies, and circadian regulation—as effective means to restore HPA axis homeostasis and mitigate the physiological impacts of chronic stress [65] [63] [67]. Future research directions should prioritize multi-omics approaches to elucidate individual differences in intervention responsiveness, longitudinal studies to establish durability of effects, and mechanistic trials to refine intervention parameters for specific clinical populations [7] [61]. The translation of these findings into clinical practice and public health initiatives holds significant potential for reducing stress-related pathology and enhancing psychological resilience across diverse populations.
Mechanisms of Dysregulation and Diagnostic-Translation Approaches
The hypothalamic-pituitary-adrenal (HPA) axis serves as the body's primary neuroendocrine stress response system, with its dysregulation representing a critical pathway through which psychological stress manifests as physiological disease. This whitepaper synthesizes current research on the spectrum of HPA axis dysfunction, progressing from initial hypercortisolism to eventual adrenal exhaustion. We examine the molecular mechanisms underlying this dysregulation, including glucocorticoid receptor resistance, impaired negative feedback, and epigenetic modifications. The clinical implications of HPA axis dysfunction extend across multiple domains including autoimmune disease development, metabolic disorders, and neuropsychiatric conditions. This review provides a comprehensive framework for researchers and drug development professionals, detailing experimental methodologies, biomarker panels, and emerging therapeutic targets aimed at restoring neuroendocrine balance.
The HPA axis constitutes a sophisticated neuroendocrine circuit involving the hypothalamus, pituitary gland, and adrenal glands, functioning as the body's central stress response system. Upon perceiving stress, hypothalamic neurons release corticotropin-releasing factor (CRF), which stimulates the anterior pituitary to secrete adrenocorticotropic hormone (ACTH). ACTH subsequently prompts the adrenal cortex to produce and release glucocorticoids—primarily cortisol in humans—into systemic circulation [17]. Cortisol then executes widespread effects by binding to glucocorticoid receptors (GRs) distributed throughout tissues including the gastrointestinal tract, immune cells, neurons, and glial cells [17]. This cascade is regulated via a negative feedback loop where elevated cortisol levels suppress further CRF and ACTH release, maintaining systemic homeostasis [17].
Chronic stress induces maladaptive changes in this finely tuned system, leading to HPA axis dysregulation. Under persistent activation, the system undergoes complex alterations including glucocorticoid receptor desensitization, impaired negative feedback mechanisms, and paradoxical cortisol dysregulation [7] [17]. The resulting hormonal imbalance manifests not as a singular entity but as a spectrum of dysfunction, initially characterized by hypercortisolism that may progress to a state of hypoactivation often described as "adrenal exhaustion" in clinical settings. This dysregulation fosters a pro-inflammatory state through weakened protective immune mechanisms and promotes cytokine imbalance, shifting the immune response toward autoimmunity [7]. Evidence from both human and animal studies associates persistent HPA dysfunction with diseases such as systemic lupus erythematosus, rheumatoid arthritis, and multiple sclerosis [7].
The Dysregulation Spectrum: From Hypercortisolism to Adrenal Exhaustion
HPA axis dysfunction progresses through identifiable stages characterized by distinct hormonal profiles and clinical manifestations. The transition through these stages represents a continuum of neuroendocrine adaptation and eventual exhaustion under chronic stress loads.
Table 1: Stages of HPA Axis Dysfunction
| Stage | Hormonal Profile | Clinical Manifestations | Neuroimmune Correlates |
|---|---|---|---|
| Alarm Stage | High cortisol output, elevated CRF and ACTH [70] | "Wired but tired" sensation, anxiety, irritability, insomnia, preserved functionality despite symptoms [70] | Initial inflammatory activation, reduced immune suppression [7] |
| Resistance Stage | Erratic cortisol secretion, fluctuating ACTH, developing glucocorticoid resistance [17] [70] | Unpredictable energy crashes, mood swings, cravings for sugar/salt, afternoon fatigue, frequent illnesses [70] | Emerging low-grade systemic inflammation, increased pro-inflammatory cytokines (IL-6, TNF-α) [17] |
| Burnout Stage | Low cortisol output, blunted ACTH response, downregulated HPA axis [17] [70] | Profound exhaustion unrelieved by sleep, apathy, anhedonia, cognitive dysfunction ("brain fog"), compromised immunity [70] | Significant immune dysregulation, heightened autoimmune susceptibility, systemic inflammation [7] |
The progression through these stages demonstrates remarkable consistency across research domains. Chronic stress leads to impaired HPA axis feedback, glucocorticoid receptor resistance, and paradoxical cortisol dysregulation [7]. The molecular underpinnings of this progression involve complex adaptations, including glucocorticoid receptor desensitization through receptor downregulation and impaired negative feedback mechanisms [17]. Emerging research also indicates that individual differences—such as genetic predisposition, early-life stress, and comorbid conditions—can further modulate HPA axis reactivity, contributing to the variability observed across studies [17].
Molecular Mechanisms and Signaling Pathways
The pathophysiological progression of HPA axis dysfunction involves sophisticated molecular mechanisms that disrupt normal neuroendocrine signaling. Chronic stress exposure induces significant alterations in glucocorticoid receptor sensitivity and function, ultimately leading to systemic dysregulation.
Glucocorticoid Receptor Resistance and Inflammatory Signaling
A fundamental mechanism in HPA axis dysregulation involves the development of glucocorticoid receptor (GR) resistance. Under conditions of chronic stress, persistent cortisol elevation leads to downregulation of GR expression and impaired receptor function [17]. This resistance disrupts the normal negative feedback loop, resulting in sustained CRF and ACTH production despite high circulating cortisol levels [17]. The molecular basis for this phenomenon involves post-translational modifications of the GR, including phosphorylation and reduced nuclear translocation, which diminish its transcriptional activity [17].
Concurrently, GR resistance creates a pro-inflammatory state by abolishing cortisol's anti-inflammatory effects. Glucocorticoids normally suppress inflammation by inhibiting pro-inflammatory transcription factors such as NF-κB and AP-1 [7]. With GR resistance, this suppression is lifted, leading to increased production of pro-inflammatory cytokines including IL-6, TNF-α, and CRP [17]. These cytokines further exacerbate HPA axis dysregulation by stimulating CRF and ACTH secretion, creating a vicious cycle of inflammation and stress hormone dysregulation [17].
HPA Axis Dysregulation in Chronic Stress: This diagram illustrates the vicious cycle of HPA axis dysregulation under chronic stress conditions, highlighting the development of glucocorticoid receptor resistance and the subsequent impairment of negative feedback mechanisms.
Epigenetic Modifications in HPA Axis Regulation
Long-term stress or chronic corticosterone exposure induces stable changes in gene expression through epigenetic mechanisms including DNA methylation, hydroxymethylation, and histone modification [17]. These changes affect genes in brain regions critical for emotion and cognition, including the hippocampus and prefrontal cortex (PFC) [17]. Research demonstrates that chronic stress and excessive glucocorticoids cause dendritic shrinkage and reduce synaptic plasticity in the hippocampus [17]. Specifically, stress-induced epigenetic modifications affect GR expression in the hippocampus, further disrupting the negative feedback loop and perpetuating HPA axis hyperactivity [17].
The timing of stress exposure is critical in programming HPA axis function. Early-life stress has particularly potent and enduring effects on DNA methylation patterns of genes regulating HPA activity, including CRF and GR genes [17]. These programmed changes create a predisposition to HPA axis dysregulation that persists throughout the lifespan and may manifest as increased vulnerability to stress-related disorders in adulthood [17].
Experimental Models and Assessment Methodologies
Rigorous experimental models are essential for investigating the complex dynamics of HPA axis dysfunction across its spectrum. The following methodologies represent current best practices in the field.
Biomarker Assessment Protocols
Comprehensive HPA axis evaluation requires multi-system biomarker assessment to capture the full extent of neuroendocrine-immune interactions.
Table 2: Key Biomarkers for HPA Axis Function Assessment
| Biomarker Category | Specific Assays | Research Utility | Technical Considerations |
|---|---|---|---|
| HPA Axis Hormones | Diurnal salivary cortisol (multiple samples), 24-hour urinary free cortisol, plasma ACTH, CRF stimulation test [71] | Maps circadian rhythm disruption, identifies hyper/hypocortisolism, localizes defect level (pituitary vs. adrenal) [47] | Strict timing for diurnal collection, standardized pre-analytical conditions, multiple sampling points essential [47] |
| Inflammatory Markers | High-sensitivity CRP, IL-6, TNF-α, multiplex cytokine panels [17] | Quantifies pro-inflammatory state linked to glucocorticoid resistance, tracks neuroimmune interactions [17] | Accounts for acute inflammation confounders, standardized processing for cytokine stability |
| Cellular & Molecular Assays | Cell-free RNA sequencing, glucocorticoid receptor expression & function assays, epigenetic profiling (DNA methylation) [72] | Reveals system-wide cellular stress responses, assesses GR resistance mechanisms, identifies epigenetic modifications [17] [72] | Advanced computational analysis for omics data, careful cell processing for receptor assays |
Cell-Free RNA Sequencing for System-Wide Stress Assessment
The analysis of cell-free RNA (cfRNA) represents a cutting-edge methodology for investigating system-wide cellular stress responses in HPA axis dysfunction. This technique leverages RNA expelled into blood plasma during cellular damage and death, providing an "activity log" of biological processes across multiple tissues [72].
Experimental Protocol:
- Sample Collection: Collect blood samples in EDTA or specialized cell-free RNA tubes followed by immediate centrifugation at 4°C (1600 × g for 10 minutes) to separate plasma from cellular components [72].
- RNA Isolation: Extract cfRNA from plasma using commercial kits with DNase treatment to remove genomic DNA contamination, incorporating synthetic spike-in RNAs for quality control and normalization [72].
- Library Preparation and Sequencing: Convert isolated RNA to cDNA followed by library preparation optimized for low-abundance transcripts. Sequence using high-throughput platforms (Illumina NovaSeq) with minimum 20 million reads per sample [72].
- Bioinformatic Analysis: Map sequences to the reference genome, quantify transcript abundances, and employ machine-learning algorithms to identify differentially expressed patterns. Deconvolve tissue origins using cell type-specific marker genes from reference databases [72].
- Validation: Confirm key findings using orthogonal methods such as qRT-PCR or digital PCR in an independent cohort [72].
This approach has demonstrated 77% accuracy in detecting chronic fatigue syndrome (a condition with documented HPA axis involvement) and identified significant differences in 700+ transcripts between patients and controls, highlighting immune dysregulation and T-cell exhaustion patterns [72].
Research Reagent Solutions
The following reagents and materials represent essential tools for investigating HPA axis dysfunction in experimental models.
Table 3: Essential Research Reagents for HPA Axis Investigation
| Reagent Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Hormone Assay Kits | Salivary cortisol ELISA, ACTH chemiluminescent immunoassay, urinary free cortisol RIA [71] | Quantifying hormonal levels across diurnal cycles, response to stressors | Select validated kits with appropriate sensitivity ranges for expected concentrations |
| Cell Culture Models | Primary adrenal cortical cells, pituitary cell lines (AtT-20), hypothalamic neuronal cells | In vitro modeling of HPA axis components, drug screening | Maintain appropriate steroid-free conditions for hormone response studies |
| Molecular Biology Reagents | GR antagonists (mifepristone), CRF receptor antagonists, epigenetic modifiers (DNA methyltransferase inhibitors) [73] | Mechanistic studies of receptor function, signaling pathways, epigenetic regulation | Include appropriate vehicle controls and dose-response designs |
| Animal Models | Chronic mild stress paradigms, early-life separation models, CRF-overexpressing transgenic mice [17] | Investigating HPA axis dysfunction progression, testing therapeutic interventions | Standardize stress protocols across experiments; consider genetic background influences |
Clinical Implications and Therapeutic Targeting
HPA axis dysregulation represents a convergent mechanism underlying multiple disease pathologies, offering promising avenues for therapeutic intervention.
Neuroimmune Connections and Autoimmune Disease
The link between HPA axis dysfunction and autoimmunity represents a particularly significant clinical implication. Chronic stress leads to impaired HPA axis feedback, glucocorticoid receptor resistance, and paradoxical cortisol dysregulation, fostering a pro-inflammatory state [7]. This dysregulation promotes cytokine imbalance, weakens protective immune mechanisms, and shifts the immune response toward autoimmunity [7]. Evidence from both human and animal studies associates persistent HPA dysfunction with diseases such as systemic lupus erythematosus, rheumatoid arthritis, and multiple sclerosis [7].
The gut-brain axis serves as a critical mediator of this stress-immune communication. Chronic stress disrupts gut microbiota composition and alters the gut-brain axis via the vagus nerve, further exacerbating stress-related mental health issues [74] [17]. Specific microbial strains (e.g., Lactobacillus reuteri) may alleviate inflammatory responses and improve stress-related behaviors by down-regulating the expression of pro-inflammatory factors (IL-6 and TNF-α) [74]. These findings highlight the potential for microbiota-targeted interventions in HPA axis-related disorders.
Pharmacological Modulation of HPA Axis Function
Current pharmacological approaches to HPA axis modulation include both conventional anxiolytics and novel targeted therapies:
Conventional Agents:
- Benzodiazepines: Reduce activity of CRF neurons in the hypothalamus, providing temporary suppression of HPA axis hyperactivity [73].
- Selective Serotonin Reuptake Inhibitors (SSRIs): The SSRI escitalopram inhibits CRF release in the central nucleus of the amygdala while increasing glucocorticoid receptor density in the hippocampus and hypothalamus [73].
- Tricyclic Antidepressants: Modulate HPA axis function through indirect mechanisms, potentially involving receptor sensitization [73].
Novel Therapeutic Approaches:
- CRF Receptor Antagonists: Target the initiating signal of the HPA axis cascade, offering potential for more specific intervention [73].
- Glucocorticoid Receptor Modulators: Selective GR modulators aim to restore receptor sensitivity and feedback regulation without complete receptor blockade [17].
- Anti-inflammatory Strategies: Targeting the inflammatory consequences of HPA dysregulation with cytokine inhibitors or anti-inflammatory drugs [17].
- Microbiota-Targeted Interventions: Probiotic supplementation, dietary interventions, and fecal microbiota transplantation to restore gut-brain axis communication [74].
The spectrum of HPA axis dysfunction, progressing from hypercortisolism to adrenal exhaustion, represents a fundamental pathway through which chronic stress disrupts physiological homeostasis and promotes disease pathogenesis. Understanding the molecular mechanisms underlying this progression—including glucocorticoid receptor resistance, epigenetic modifications, and neuroimmune interactions—provides critical insights for researchers and drug development professionals. The experimental methodologies and reagent solutions detailed in this review offer practical tools for advancing investigation in this field. Future research directions should focus on multi-omics approaches to clarify the reversibility of HPA alterations, identify resilience factors, and develop targeted interventions that restore neuroendocrine balance across the dysfunction spectrum.
Glucocorticoid receptor (GR) resistance represents a critical breakdown in hypothalamic-pituitary-adrenal (HPA) axis signaling, characterized by reduced tissue sensitivity to glucocorticoids despite adequate or elevated circulating hormone levels. This comprehensive review synthesizes current understanding of the molecular mechanisms underpinning GR resistance, encompassing GR gene mutations, alternative splicing variants, post-translational modifications, and alterations in chromatin remodeling complexes. We examine the systemic consequences of impaired GR signaling across multiple physiological domains, including immune dysregulation, metabolic disturbances, and neuroendocrine pathologies. The clinical implications span rare genetic syndromes, inflammatory diseases, hematological malignancies, and psychiatric disorders, presenting significant challenges for therapeutic management. Emerging strategies targeting GR resistance mechanisms offer promising avenues for restoring glucocorticoid sensitivity and improving treatment outcomes across diverse disease contexts.
Glucocorticoids (GCs) are steroid hormones that regulate essential physiological processes including development, homeostasis, metabolism, cognition, and inflammation through the ubiquitously expressed glucocorticoid receptor (GR) [75]. The human GR (NR3C1) is located on chromosome 5q31-32 and consists of nine exons that give rise to multiple isoforms through alternative splicing and translational initiation [75] [76]. GR functions as a ligand-dependent transcription factor with modular organization containing an N-terminal transactivation domain (AF-1), a central DNA-binding domain (DBD) with two zinc finger motifs, and a C-terminal ligand-binding domain (LBD) that includes the AF-2 activation function [75].
In the classic signaling paradigm, unliganded GR resides in the cytoplasm as part of a heterocomplex with chaperone proteins (HSP90, HSP70, HSP40, p23) and immunophilins (FKBP51, FKBP52) [75] [76]. Upon glucocorticoid binding, GR undergoes conformational changes, dissociates from the chaperone complex, homodimerizes, and translocates to the nucleus where it binds glucocorticoid response elements (GREs) to transactivate or transrepress target genes [75]. GR can also regulate gene expression through protein-protein interactions with other transcription factors like NF-κB and AP-1, a mechanism known as "tethering" [76].
Glucocorticoid resistance is defined as reduced or impaired GR responsiveness to endogenous or synthetic glucocorticoids, leading to dysregulated HPA axis feedback, elevated cortisol levels, and clinical manifestations of impaired glucocorticoid signaling despite adequate hormone production [77] [78]. This resistance exists on a spectrum from partial to complete and may be generalized or tissue-specific, contributing to numerous pathological conditions.
Molecular Mechanisms of Glucocorticoid Receptor Resistance
Genetic Alterations in the Glucocorticoid Receptor
The NR3C1 gene encoding GR spans approximately 80 kb and contains 9 exons. Multiple mechanisms at the genetic level contribute to glucocorticoid resistance:
Table 1: Genetic Mechanisms of Glucocorticoid Resistance
| Mechanism | Molecular Consequence | Functional Impact |
|---|---|---|
| Loss-of-function mutations | Impaired ligand binding, nuclear translocation, or DNA binding | Reduced transactivation capacity [77] |
| Alternative splicing | Altered GR isoform expression (GRβ, GRγ, GR-A, GR-P) | Dominant-negative effects; altered transcriptional activity [75] [76] |
| Alternative translation initiation | Generation of N-terminal truncated isoforms (GR-A, B, C1-C3, D1-D3) | Differential regulation of gene subsets [75] |
| Promoter polymorphisms | Altered GR expression levels | Tissue-specific sensitivity changes [75] |
Generalized glucocorticoid resistance syndrome is a rare disorder caused by loss-of-function mutations in NR3C1. A systematic review of 71 patients identified 48 distinct mutations, with heterozygous mutations representing 78.9% of cases and homozygous/compound heterozygous mutations comprising 21.1% [77]. These mutations distribute throughout the receptor: 29.2% in the N-terminal domain, 25% in the DNA-binding domain, 35.4% in the ligand-binding domain, and 10.4% in the hinge region [77]. Patients with homozygous/compound heterozygous mutations present with more severe manifestations including early-onset hypertension (86% vs. 46% in heterozygotes) and hypokalemia (71% vs. 25%) [77].
The GRβ isoform, which differs in the C-terminal 50 amino acids and cannot bind glucocorticoids, exerts dominant-negative effects on GRα transactivation when expressed at sufficient levels [75]. Similarly, GRγ contains a single amino acid insertion in the DBD that reduces transactivation potency by approximately 50% [76]. In malignant cells, alternative splicing generates GR-A and GR-P variants lacking functional N- and C-terminal domains, respectively [76].
Post-Translational Modifications and Coregulator Dynamics
GR function is modulated by various post-translational modifications (PTMs) including phosphorylation, acetylation, ubiquitination, and SUMOylation, primarily within the N-terminal domain [76]. These PTMs influence GR stability, subcellular localization, protein-protein interactions, and transcriptional activity. For instance, phosphorylation at specific serine residues modulates GR transcriptional activity and target gene specificity [76].
The coregulator balance profoundly impacts GR signaling. Coactivators (SRC-1, GRIP1, CBP/p300) enhance GR transactivation, while corepressors (NCoR1, SMRT) attenuate signaling [75]. In corticotroph tumors, downregulation of BRG1 and HDAC2—components of the GR transrepression complex—compromises glucocorticoid-mediated repression of POMC transcription, contributing to glucocorticoid resistance in Cushing's disease [79].
Table 2: Experimental Assessment of GR Resistance Mechanisms
| Experimental Approach | Methodology | Key Reagents |
|---|---|---|
| GR expression analysis | Western blot, immunohistochemistry, flow cytometry | Anti-GR antibodies (multiple clones for different epitopes) |
| GR functional assays | Luciferase reporter assays with GRE-driven constructs | GRE-luciferase plasmids, glucocorticoid analogs |
| Ligand binding studies | Whole-cell or cytosolic radioligand binding assays | [3H]-dexamethasone, RU486 for competition studies |
| Nuclear translocation | Immunofluorescence, GFP-GR fusion constructs | Fluorescent tags, nuclear markers, live-cell imaging systems |
| Gene expression profiling | RNA sequencing, RT-qPCR of GC-responsive genes | Primers for GILZ, FKBP5, SGK1 |
| Chromatin accessibility | ChIP-seq, ATAC-seq, DNase hypersensitivity assays | Anti-GR antibodies, sequencing reagents |
Altered Chromatin Landscape and Epigenetic Regulation
The chromatin environment significantly influences GR signaling through mechanisms that modulate DNA accessibility and receptor binding dynamics. Research reveals that GR binding to chromatin is highly dynamic, with rapid cycling on and off chromatin occurring within seconds to minutes in living cells [75]. Tissue-specific target gene activation by glucocorticoids depends on chromatin accessibility at GR-binding sites, which is determined by DNA methylation patterns and higher-order chromatin structures [75].
In lymphoid malignancies, changes in chromatin remodeling complexes and histone modifications contribute to therapy resistance. For instance, reduced expression of chromatin remodelers like BRG1 compromises GR-mediated transrepression of pro-survival genes [80]. Additionally, DNA methylation of specific GREs can prevent GR binding and target gene activation, establishing epigenetic mechanisms of resistance [75].
Signaling Pathway Interplay in Glucocorticoid Resistance
The following diagram illustrates key molecular pathways and their interactions in glucocorticoid resistance:
Figure 1: Molecular Pathways in Glucocorticoid Resistance. This diagram illustrates the complex interplay between glucocorticoid signaling and resistance mechanisms. Glucocorticoid binding to GR leads to target gene regulation, including induction of DUSP proteins that inhibit MAPK pathways. Resistance arises through multiple mechanisms including NR3C1 mutations, altered GR isoforms, coregulator imbalance, and chromatin remodeling. Activation of NF-κB and MAPK signaling pathways further promotes glucocorticoid resistance.
Cross-Talk with MAPK Signaling Pathways
The mitogen-activated protein kinase (MAPK) pathways represent critical modulators of GR function. Chronic inflammation leads to sustained MAPK activation, which phosphorylates GR and coregulators, altering their function and contributing to glucocorticoid resistance [76]. Specifically, excessive activation of JNK and p38 MAPK pathways promotes GR phosphorylation at inhibitory sites, reducing nuclear translocation and DNA-binding capacity [76].
Dual-specificity phosphatases (DUSPs), particularly DUSP1 (MKP-1), function as key negative regulators of MAPK signaling and are induced by glucocorticoids as part of their anti-inflammatory mechanism [76]. In conditions of glucocorticoid resistance, impaired DUSP induction fails to adequately suppress MAPK signaling, creating a vicious cycle of inflammation and resistance. This mechanism is particularly relevant in chronic inflammatory diseases where approximately 30% of glucocorticoid-treated patients develop resistance [76].
HSP90 Chaperone Complex and Receptor Maturation
The HSP90 chaperone complex is essential for maintaining GR in a high-affinity ligand-binding conformation. HSP90, along with co-chaperones including FKBP51 and FKBP52, facilitates proper GR folding and maturation [79]. FKBP51 overexpression stabilizes GR in a low-affinity state, while FKBP52 promotes high-affinity binding and nuclear translocation [79]. An elevated FKBP51/FKBP52 ratio creates a predisposition to glucocorticoid resistance.
In corticotroph tumors, HSP90 is overexpressed compared to normal pituitary tissue, potentially contributing to glucocorticoid resistance through altered GR folding dynamics [79]. Pharmacological inhibition of HSP90 restores glucocorticoid sensitivity in experimental models, highlighting the therapeutic potential of targeting the chaperone system [79].
Systemic Consequences of Glucocorticoid Resistance
Neuroendocrine and Psychiatric Manifestations
Glucocorticoid resistance significantly impacts HPA axis function, disrupting the delicate balance of neuroendocrine signaling. In generalized glucocorticoid resistance syndrome, impaired GR signaling leads to compensatory HPA axis activation with elevated ACTH and cortisol levels [77]. Despite hypercortisolism, patients typically lack Cushingoid features and may instead present with manifestations of mineralocorticoid and androgen excess, including hypertension, hypokalemia, and precocious puberty [77].
In major depressive disorder, glucocorticoid resistance manifests as immune dysregulation with elevated pro-inflammatory cytokines [78]. Meta-analyses reveal that depressed patients with the highest degrees of glucocorticoid resistance (hypercortisolemia) show significantly increased levels of IL-6 (d = 0.94; 95% CI 0.29-1.59) and TNF-α (d = 0.46; 95% CI 0.12-0.79) compared to those with normal HPA axis function [78]. This combination of glucocorticoid resistance and inflammation contributes to neuroendocrine-immune imbalance in mood disorders.
Chronic stress leads to HPA axis dysregulation through impaired GR-mediated negative feedback, resulting in sustained cortisol elevation and potential hippocampal atrophy [15]. The gut-brain axis further modulates this relationship, as gut dysbiosis increases intestinal permeability, allowing endotoxins to enter circulation and promote systemic inflammation that exacerbates glucocorticoid resistance [15].
Inflammatory and Autoimmune Diseases
In chronic inflammatory conditions such as rheumatoid arthritis, asthma, and chronic obstructive pulmonary disease (COPD), glucocorticoid resistance presents a major therapeutic challenge. The prevalence of resistance varies by disease, affecting approximately 30% of rheumatoid arthritis patients, 4-10% of asthma patients, and nearly all COPD and sepsis patients [76].
At the molecular level, inflammation-induced glucocorticoid resistance involves activation of pro-inflammatory transcription factors (NF-κB, AP-1) that directly interfere with GR signaling through protein-protein interactions [76]. Additionally, increased expression of the GRβ isoform in inflammatory cells creates a pool of dominant-negative receptors that further compromise glucocorticoid responsiveness [75]. This resistance mechanism is particularly prominent in severe asthma, where airway cells exhibit elevated GRβ expression [75].
Hematological Malignancies
Glucocorticoid resistance represents a significant obstacle in treating lymphoid malignancies, particularly acute lymphoblastic leukemia (ALL), where 10-30% of patients exhibit poor response to glucocorticoid therapy [76] [80]. In childhood ALL, the prednisone response after 7 days of monotherapy serves as a key prognostic factor for treatment adaptation [80].
Multiple mechanisms contribute to therapy resistance in hematological cancers:
- Reduced GR expression: Downregulation of GR protein levels diminishes cellular sensitivity to glucocorticoids [80]
- Altered GR isoform ratio: Increased expression of inactive GR variants compromises transcriptional activity [80]
- Dysregulated apoptosis pathways: Imbalance in BCL-2 family proteins prevents glucocorticoid-induced cell death [80]
- Kinase pathway activation: Aberrant signaling through PI3K/AKT, JAK/STAT, and MAPK pathways interferes with GR function [80]
In chronic lymphocytic leukemia (CLL), high-dose methylprednisolone can overcome resistance by suppressing Wnt signaling through downregulation of LEF-1, a critical survival factor in CLL cells [80].
Research Reagent Solutions for Investigating GR Resistance
Table 3: Essential Research Reagents for Glucocorticoid Resistance Studies
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| GR Ligands | Dexamethasone, Prednisolone, Cortisol, RU486 | Receptor activation, competition assays |
| GR Antibodies | Anti-GR monoclonal antibodies (clone 4H2 for N-terminus, clone 5E4 for DBD) | Western blot, immunohistochemistry, ChIP |
| GR Expression Vectors | Wild-type GRα, GRβ, GR mutants, GFP-GR fusions | Functional rescue experiments, localization studies |
| Signaling Inhibitors | MAPK inhibitors (SB203580, U0126), HSP90 inhibitors (17-AAG) | Pathway modulation, combination therapies |
| Cytokine Assays | IL-6, TNF-α ELISA kits, multiplex bead arrays | Inflammation monitoring, cytokine profiling |
| Apoptosis Detection | Annexin V staining, caspase activity assays | Cell death quantification in malignancies |
Experimental Approaches for Assessing GR Function
Methodologies for Evaluating GR Signaling
The following diagram outlines a comprehensive experimental workflow for investigating glucocorticoid resistance mechanisms:
Figure 2: Experimental Workflow for GR Resistance Investigation. This comprehensive workflow outlines key methodologies for assessing glucocorticoid receptor function and identifying resistance mechanisms. The approach integrates GR expression analysis, functional assays, genomic profiling, and parallel investigations of genetic and epigenetic modifications.
In Vitro Assessment of GR Transactivation Capacity
Protocol: GRE-Luciferase Reporter Assay
- Cell Seeding: Plate appropriate cell line (e.g., HEK293, A549) in 24-well plates at 5×10^4 cells/well and culture for 24 hours
- Transfection: Co-transfect with:
- 400 ng GRE-luciferase reporter plasmid
- 100 ng GR expression vector (or empty vector control)
- 50 ng Renilla luciferase control plasmid (transfection normalization)
- Treatment: 24 hours post-transfection, treat with vehicle or glucocorticoids (e.g., 100 nM dexamethasone) for 16-24 hours
- Luciferase Assay: Lyse cells and measure firefly and Renilla luciferase activities using dual-luciferase reporter assay system
- Data Analysis: Normalize firefly luciferase values to Renilla controls and express as fold induction over vehicle-treated cells
Expected Outcomes: Glucocorticoid-sensitive cells typically show 5-20 fold induction, while resistant cells demonstrate significantly reduced induction (≤2 fold) [75] [80].
GR Nuclear Translocation Quantification
Protocol: Immunofluorescence and Image Analysis
- Cell Culture: Seed cells on glass coverslips and culture until 60-70% confluent
- Treatment: Stimulate with 100 nM dexamethasone for various time points (0, 15, 30, 60, 120 min)
- Fixation: Rinse with PBS and fix with 4% paraformaldehyde for 15 minutes at room temperature
- Permeabilization and Blocking: Permeabilize with 0.2% Triton X-100 for 10 minutes, block with 5% BSA for 1 hour
- Immunostaining: Incubate with anti-GR primary antibody (1:200) overnight at 4°C, followed by fluorescent secondary antibody (1:500) for 1 hour at room temperature
- Nuclear Staining: Counterstain with DAPI (1 μg/mL) for 5 minutes
- Imaging and Analysis: Acquire images by confocal microscopy and quantify nuclear/cytoplasmic fluorescence intensity using ImageJ software
Scoring System: Calculate nuclear translocation ratio (mean nuclear intensity/mean cytoplasmic intensity). Values >2.0 indicate robust translocation, while values <1.5 suggest impaired nuclear translocation [75] [80].
Glucocorticoid receptor resistance represents a multifactorial phenomenon with diverse molecular origins and profound systemic consequences. The intricate interplay between genetic predisposition, signaling pathway cross-talk, epigenetic modifications, and inflammatory mediators creates a complex resistance landscape that varies across tissues and disease states. Understanding these mechanisms is paramount for developing targeted strategies to restore glucocorticoid sensitivity and improve therapeutic outcomes.
Future research directions should focus on multi-omics approaches to comprehensively characterize resistance signatures, advanced imaging techniques to visualize GR dynamics in real-time, and novel combinatorial therapies that simultaneously target multiple resistance mechanisms. The development of selective glucocorticoid receptor modulators (SGRMs) with improved therapeutic indices and tissue-specific actions holds particular promise for overcoming resistance while minimizing adverse effects.
As our understanding of glucocorticoid receptor biology continues to evolve, so too will our ability to diagnose, monitor, and therapeutically address glucocorticoid resistance across the spectrum of neuroendocrine, inflammatory, and neoplastic diseases.
Autoimmune diseases and central nervous system (CNS) disorders represent a significant burden in global healthcare, characterized by complex pathogeneses involving genetic, epigenetic, and environmental factors. Among these factors, chronic stress has emerged as a critical modifier of immune regulation, primarily through its impact on the hypothalamic-pituitary-adrenal (HPA) axis [81]. The HPA axis serves as the principal neuroendocrine pathway through which stress alters immune responses, mainly via glucocorticoid secretion [81]. This review synthesizes current literature on HPA axis physiology, the mechanisms of cortisol signaling, and the maladaptive effects of chronic stress, with emphasis on clinical and experimental findings linking HPA dysfunction to immune imbalance and neuroinflammation. Understanding these pathways provides opportunities for therapeutic interventions and identifies key areas for future research focused on multi-omics and longitudinal approaches to clarify the reversibility of HPA alterations and identify resilience factors [81].
The Physiology of the HPA Axis and Cortisol
The hypothalamic-pituitary-adrenal (HPA) axis is a neuroendocrine system comprising hormones, signaling pathways, and feedback loops that regulate various physiological processes, with stress response being one of its primary functions [81]. This response begins in the paraventricular nucleus (PVN) of the hypothalamus with the release of corticotropin-releasing hormone (CRH). CRH then acts on the anterior pituitary gland to stimulate the secretion of adrenocorticotropic hormone (ACTH), which subsequently travels through the bloodstream to the adrenal cortex, specifically targeting the zona fasciculata to induce cortisol production [81].
Cortisol, a glucocorticoid hormone, is secreted in a basal state following a pulsatile and oscillatory pattern according to the circadian rhythm, with surges occurring in response to stressful stimuli [81]. The physiological responses to cortisol depend on the specific organ or system involved. At the immune system level, cortisol's anti-inflammatory properties are well-established and utilized in clinical settings. It enhances innate immune responses while simultaneously reducing cytokine expression and production [81]. Cortisol exerts its effects through the glucocorticoid receptor (GR), which modulates gene expression by suppressing pro-inflammatory signaling pathways involving transcription factors such as NF-κB and AP-1, resulting in decreased production of pro-inflammatory cytokines (including IL-1β, IL-6, and TNF-α), chemokines, and other immune-activating molecules [81].
Table 1: Key Components of the HPA Axis and Their Functions
| Component | Location | Primary Function | Key Secretions |
|---|---|---|---|
| Paraventricular Nucleus (PVN) | Hypothalamus | Initiates stress response; integrates neural signals | Corticotropin-Releasing Hormone (CRH) |
| Anterior Pituitary | Brain Base | Relays hormonal signals to periphery | Adrenocorticotropic Hormone (ACTH) |
| Adrenal Cortex | Adrenal Glands | Final endocrine effector of HPA axis | Cortisol (primary glucocorticoid) |
| Hippocampus | Medial Temporal Lobe | High GR density; central to negative feedback inhibition | - |
| Amygdala | Temporal Lobe | Processes emotional stressors; activates PVN | - |
The HPA axis is regulated by a precise negative feedback mechanism wherein both ACTH and cortisol act as inhibitors of CRH and ACTH secretion, thereby maintaining homeostasis [81]. This orchestrated system enables the body to mount an adequate response to stressful stimuli while preventing excessive activation. However, under conditions of prolonged stress, persistent elevation of cortisol can disrupt this regulatory system, leading to hypersecretion, sensitized stress responses, and potential adrenal exhaustion [81].
Chronic Stress and HPA Axis Dysregulation
The persistent activation of the HPA axis caused by chronic stress alters normal regulatory processes, including loss of the normal pulsatile and circadian rhythms, impaired negative feedback mechanisms, and maladaptive changes in receptor sensitivity [81]. Over time, this dysregulation can lead to adrenal hypertrophy and increased hormonal secretion, as demonstrated in animal models [81]. Excess cortisol affects multiple structures, including key neuroanatomical sites such as the hippocampus and prefrontal cortex, where downregulation of glucocorticoid receptor (GR) density and impaired feedback inhibition further perpetuate HPA axis dysregulation [81].
A critical consequence of chronic HPA axis activation is the development of glucocorticoid receptor resistance, wherein immune cells become less responsive to the suppressive effects of cortisol [81]. This resistance creates a pro-inflammatory state despite elevated circulating cortisol levels. Furthermore, the initial state of hypercortisolism may evolve into a paradoxical hypocortisolism state in advanced or prolonged stress exposure due to adrenal resistance and impaired signaling within the HPA axis [81] [82]. This functional impairment, sometimes referred to as adrenal exhaustion, reflects the diminished responsiveness of the adrenal glands to regulatory stimuli [81].
The transition from adaptive stress responses to maladaptive HPA axis dysfunction follows a multi-stage process:
Diagram 1: Transition from acute stress adaptation to chronic HPA axis dysfunction leading to neuroinflammation. GR = Glucocorticoid Receptor.
These HPA axis alterations have significant clinical implications. Hypocortisolism and glucocorticoid resistance can impair multiple physiological systems and functions, increasing vulnerability to inflammatory or autoimmune diseases due to inadequate glucocorticoid-mediated immune regulation [81]. The paradoxical cortisol dysregulation under chronic stress creates a mechanistic bridge between psychological stress and physical disease pathology, particularly in the CNS.
Immunological Consequences of HPA Axis Dysfunction
The pulsatile, circadian rhythm of cortisol release plays a crucial role in synchronizing immune responses and maintaining homeostasis. Under conditions of chronic stress, HPA axis dysregulation leads to an altered cortisol response that impairs effective immune regulation, resulting in sustained production of pro-inflammatory cytokines like IL-6 and TNF-α [81]. A study examining parents of cancer patients demonstrated that chronic psychological stress significantly reduced dexamethasone's ability to suppress IL-6 production compared to parents of medically healthy children, providing direct evidence of impaired glucocorticoid-mediated immune regulation under chronic stress conditions [81].
The cytokine imbalance resulting from HPA axis dysfunction creates a pro-inflammatory environment that promotes autoimmunity and neuroinflammation. Additionally, excess cortisol may increase binding to mineralocorticoid receptors (MR), which can produce a pro-inflammatory response in certain immune cell populations [81]. Mineralocorticoid receptor activation in macrophages and other immune cells promotes upregulation of genes encoding cytokines like IL-6 and TNF-α, further exacerbating the inflammatory state [81].
Table 2: Cytokine Profiles in Acute vs. Chronic Stress Conditions
| Cytokine/Cell Type | Acute Stress Response | Chronic Stress Response | Functional Consequences |
|---|---|---|---|
| IL-6 | Transient increase; suppressed by cortisol | Sustained elevation; cortisol resistance | Chronic inflammation; B-cell differentiation |
| TNF-α | Suppressed by cortisol action | Elevated due to GR resistance | Enhanced tissue inflammation; cytotoxicity |
| IL-1β | Regulated increase | Dysregulated production | Pyrogenic; promotes leukocyte recruitment |
| IL-10 | Upregulated | Suppressed | Loss of anti-inflammatory regulation |
| Microglial Activity | Context-dependent activation | Sustained activation (20-200% increase) | Synaptic pruning defects; excitotoxicity [83] |
The impact of chronic stress on neuroinflammation is particularly significant. A systematic review of preclinical studies found that psychosocial stressors consistently lead to elevated microglial activity, with increases of between 20% and 200% reported in the hippocampus across all 11 studies examining this region [83]. Approximately 75% of studies examining the prefrontal cortex found that psychosocial stress resulted in elevated Iba-1 (a microglial marker) activity, with elevations also consistently observed in the nucleus accumbens and, under some stress conditions, in the amygdala and paraventricular nucleus [83]. These effects were seen with early-life/prenatal stress as well as stressors in adulthood, supporting the "two-hit" hypothesis that proposes early-life stress primes microglia, leading to a potentiated response to subsequent stress [83].
Neuroinflammation as a Pathogenic Bridge to CNS Disorders
Neuroinflammation represents the innate and adaptive immune responses initiated toward various harmful insults through the release of inflammatory mediators by various immune cells [84]. While neuroinflammation in its initial stage is mainly beneficial and protective, prolonged or excessive inflammation serves as a pivotal pathological driver of several neurological disorders [84]. Evidence from both clinical and experimental studies indicates that neuroinflammation is the common mechanism connecting ischemic, degenerative, traumatic, demyelinating, epileptic, and psychiatric pathologies [84].
In neurodegenerative diseases, including Alzheimer's disease, Parkinson's disease, and Amyotrophic lateral sclerosis, inflammation is not only a result of neurodegeneration but also a crucial player in the disease process [85]. Protein aggregates, a common pathological phenomenon in neurodegeneration, can induce neuroinflammation which further aggravates protein aggregation and neurodegeneration. Notably, inflammation may occur earlier than detectable protein aggregation, suggesting that neuroinflammation induced by genetic variations in CNS cells or by peripheral immune cells may induce protein deposition in susceptible populations [85].
The relationship between stress-induced HPA axis dysfunction and neuroinflammation creates a vicious cycle that propagates CNS pathology. Stressors activate microglia and astrocytes, leading to excessive production of pro-inflammatory cytokines including IL-1β, IL-6, and TNF-α, chemokines such as CCL2 and CCL5, and secondary messengers including nitric oxide (NO) and reactive oxygen species (ROS) [86]. These inflammatory mediators contribute to the development of neurological symptoms by affecting brain tissue, modulating neurotransmitter systems, and triggering neurotoxic processes [86]. The impact is particularly pronounced in emotional regulation areas such as the prefrontal cortex and amygdala, which are directly affected by overactivation of cytokine networks [86].
Diagram 2: Signaling pathways linking HPA dysfunction through microglial activation to CNS pathology. GR = Glucocorticoid Receptor.
The role of neuroinflammation in epilepsy provides a compelling example of this pathway. Evidence indicates that repeated exposure to acute stress, particularly in early life, alters HPA axis function, exacerbates hippocampal sclerosis, and enhances vulnerability to epileptogenesis [84]. The stress-induced neuroinflammation, in association with dysfunction of various neurotransmitters, glucocorticoid receptors, and different neurotrophic factors, could aggravate the established pro-inflammatory effects of seizures and lead to enhanced neuronal network excitability [84]. Based on evidence of a potential correlation between stress-induced inflammation and epilepsy, researchers have emphasized the importance of early interventions for both acute and chronic stress in improving diagnosis, therapy, and outcomes for patients with epilepsy, particularly those with psychiatric comorbidities [84].
Experimental Models and Methodologies
Preclinical Stress Models
Research into stress-induced neuroinflammation has utilized various well-established preclinical models to investigate the effects of psychosocial stressors on neuroimmune parameters. These models have been validated as effective preclinical representations of the social stressors associated with increased risk of mental illness in humans [83]. The most commonly employed models include chronic restraint stress, social isolation, repeated social defeat, and early-life/prenatal stress paradigms.
Table 3: Preclinical Stress Models and Methodological Parameters
| Stress Model | Species Used | Stress Duration | Key Physiological Readouts | Neuroinflammatory Markers |
|---|---|---|---|---|
| Chronic Restraint | Rats, Mice, Gerbils | 14-21 days (up to 6h/day) | Adrenal hypertrophy, Weight changes | Iba-1 ↑ (20-200%), MHC-II ↑, CD68 ↑ |
| Social Defeat | Mice, Rats | 5-10 days (continuous or episodic) | Social avoidance, Anhedonia | Microglial priming, IL-6 ↑, TNF-α ↑ |
| Social Isolation | Mice, Rats | 2-8 weeks (continuous) | Anxiety-like behaviors, Cognitive deficits | Hippocampal Iba-1 ↑, Prefrontal cortex Iba-1 ↑ |
| Early Life Stress | Rats, Mice | Prenatal or postnatal periods | Altered HPA reactivity in adulthood | Microglial sensitization, Enhanced cytokine response to secondary challenge |
| Foot Shock | C57Bl/6 mice | 5 days (120 shocks/session) | Fear conditioning, Autonomic activation | Regional microglial activation |
The chronic restraint model involves placing animals within restrictive wire mesh or Plexiglas environments for up to 6 hours daily over a stress duration of 14-21 days [83]. Social defeat stress exposes experimental animals to aggressive residents for brief periods followed by sensory contact, inducing psychosocial stress. Social isolation involves housing social species individually for extended periods, while early-life stress paradigms include maternal separation or prenatal stress exposure [83].
Assessment Techniques
The evaluation of neuroinflammatory responses in these models relies on multiple assessment techniques, including histological analysis, molecular biology approaches, and behavioral testing. Ionized calcium binding adaptor molecule 1 (Iba-1) has been widely used as a histological microglial marker as its expression is specific and is expressed by both reactive and quiescent microglial cells [83]. Additional markers include CD68 (involved in phagocytosis), CD11b (complement receptor 3 regulating leukocyte adhesion and migration), CD45 (modulating activation and proliferation of inflammatory cell types), MHC-II (role in antigen presentation to T cells), and various pro-inflammatory cytokines including IL-1β, TNF-α, and IL-6 [83].
Morphological analysis of microglia provides additional important information. In the healthy adult central nervous system, microglia have a ramified morphology characterized by long, thin processes that enable them to search the local environment [83]. When responding to insults, the processes retract, and the cell body enlarges, giving microglia an amoeboid shape. Chronic inflammatory states are associated with a hypertrophic branch morphology with an enlarged soma [83].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Investigating Stress-Induced Neuroinflammation
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Microglial Markers | Iba-1, CD11b, CD68, TMEM119 | Identification and quantification of microglial cells | Iba-1 is expressed by both resting and activated microglia; suitable for general microglial visualization |
| Activation Panel | MHC-II, CD45, CD40, CD86 | Differentiation of microglial activation states | CD45low indicates resident microglia; CD45high indicates peripheral monocytes |
| Cytokine Panel | IL-1β, IL-6, TNF-α, IL-10, IL-4 | Quantification of pro- vs anti-inflammatory milieu | Multiplex immunoassays recommended for comprehensive profiling; species-specific reagents required |
| GR Signaling Assays | Phospho-GR antibodies, GRE-luciferase reporters, GR antagonists (RU486) | Assessment of glucocorticoid receptor function | Nuclear translocation assays critical for determining GR activity |
| HPA Axis Hormones | CORT ELISA (corticosterone), ACTH ELISA, CRH RIA | Quantification of hormonal stress response | Consider circadian rhythms in sampling; serial measurements often necessary |
| Neurodegeneration Markers | Aβ antibodies, p-Tau antibodies, α-synuclein antibodies, GFAP | Evaluation of downstream neurodegenerative effects | Context-dependent based on disease model being studied |
This toolkit enables researchers to comprehensively evaluate the multiple dimensions of stress-induced neuroinflammation, from initial HPA axis dysregulation to subsequent neuroimmune activation and eventual CNS pathology. The selection of appropriate reagents and methodologies depends on the specific research questions, model systems, and analytical approaches being employed.
The evidence synthesized in this review demonstrates that stress-induced neuroinflammation represents a critical mechanistic bridge between HPA axis dysfunction and CNS pathology. Chronic stress leads to impaired HPA axis feedback, glucocorticoid receptor resistance, and paradoxical cortisol dysregulation, which collectively foster a pro-inflammatory state in the central nervous system [81]. This neuroinflammatory environment, characterized by microglial activation and elevated pro-inflammatory cytokines, contributes to the pathogenesis of diverse neurological and psychiatric disorders, including neurodegenerative diseases, epilepsy, and major depressive disorder [84] [85] [86].
Understanding these pathways provides important opportunities for therapeutic interventions, including stress management, lifestyle modification, and neuroendocrine-targeted treatments [81]. Future research should focus on multi-omics and longitudinal approaches to clarify the reversibility of HPA alterations and identify resilience factors that might protect against stress-induced neuroinflammation [81]. The continued elucidation of these complex neuroimmune interactions will be essential for developing more effective preventive and treatment strategies for the myriad CNS disorders in which stress and inflammation play a pathogenic role.
A compelling body of evidence demonstrates that adverse early-life experiences program physiological systems toward pathological trajectories, increasing susceptibility to chronic diseases in adulthood. This whitepaper examines the maladaptive programming of the hypothalamic-pituitary-adrenal (HPA) axis and associated neuroendocrine interactions as a central mechanism linking early life stress (ELS) to later disease vulnerability. Drawing from current research, we analyze how stress during critical developmental windows reprograms stress response circuitry, induces glucocorticoid dysregulation, and triggers systemic inflammatory cascades that manifest decades later as metabolic, autoimmune, neuropsychiatric, and cardiovascular disorders. The clinical implications for drug development and novel therapeutic targets are discussed, with particular focus on timing interventions during sensitive developmental periods.
The Developmental Origins of Health and Disease paradigm posits that environmental exposures during sensitive developmental periods program an individual's physiological responses, creating permanent vulnerabilities to disease. Within this framework, early life stress—encompassing prenatal stress, childhood maltreatment, neglect, and adversity—has emerged as a potent programming stimulus that alters the trajectory of neurological, endocrine, and immune development. The HPA axis serves as the primary neuroendocrine mediator between adverse experiences and physiological dysregulation, with ELS inducing functional and structural changes that persist throughout the lifespan.
Massimo Fagioli's Human Birth Theory further conceptualizes that while birth itself is healthy and equal for all, mental illness develops exclusively in the postnatal period due to relational quality in the first year of life [87]. This aligns with broader evidence that early-life experiences shape individual responses to chronic stress and stress-related diseases during adult life, with epigenetic mechanisms serving as the molecular interface between environment and gene expression [87].
Neuroendocrine Programming: The HPA Axis as Central Mediator
HPA Axis Physiology and Developmental Trajectories
The HPA axis represents the body's central stress response system, coordinating neuroendocrine adaptations to maintain homeostasis. Upon stress exposure, corticotropin-releasing factor from the hypothalamus stimulates pituitary adrenocorticotropic hormone release, which triggers glucocorticoid production from the adrenal cortex. In humans, the primary glucocorticoid is cortisol, which regulates energy metabolism, immune function, and inflammatory responses while providing negative feedback to terminate the stress response.
During early development, the HPA axis undergoes sensitive organizational periods when its setpoints are established. Early life stress during these windows programs the system toward hyper- or hypo-reactivity, altering an individual's stress response phenotype permanently. Clinical and preclinical studies demonstrate that ELS produces lasting hyper-responsiveness to stress with exaggerated circulating glucocorticoids and enhanced anxiety-like behaviors [88]. Conversely, some individuals exhibit HPA axis hypo-activity following ELS, potentially representing a compensatory adaptation to chronic stress exposure [89].
Mechanisms of HPA Axis Programming
The programming effects of ELS on the HPA axis occur through multiple interconnected mechanisms:
Glucocorticoid Receptor Alterations: ELS induces epigenetic modifications that alter glucocorticoid receptor expression and sensitivity, particularly in the hippocampus, impairing negative feedback efficiency [88] [17].
Neuroendocrine Circuitry Remodeling: Stress during development causes dendritic shrinkage and reduces synaptic plasticity in stress-regulatory brain regions including the hippocampus, prefrontal cortex, and amygdala [17].
Gene Expression Reprogramming: Prolonged stress alters gene expression directly through glucocorticoid-driven transcription and indirectly via epigenetic modifications including DNA methylation, hydroxymethylation, and histone modification [17].
Table 1: HPA Axis Dysregulation Patterns Following Early Life Stress
| Pattern | Cortisol Profile | Stress Response | Associated Outcomes |
|---|---|---|---|
| Hyperactive HPA | Elevated basal cortisol, enhanced CAR | Exaggerated cortisol response | Depression, anxiety disorders, metabolic syndrome [89] |
| Hypoactive HPA | Low basal cortisol, flattened diurnal rhythm | Blunted cortisol response | Atypical depression, fatigue syndromes, comorbid inflammation [89] |
| Disorganized HPA | Irregular patterns, poor recovery | Inconsistent responses | Mixed psychiatric presentations, severe functional impairment |
Beyond the HPA Axis: Systemic Pathophysiological Consequences
Neuroimmune Dysregulation and Inflammation
The neuroimmune interface represents a critical pathway through which ELS exerts enduring effects on health. Chronic stress leads to impaired HPA axis feedback, glucocorticoid receptor resistance, and paradoxical cortisol dysregulation, fostering a pro-inflammatory state [7]. This dysregulation promotes cytokine imbalance, weakens protective immune mechanisms, and shifts the immune response toward autoimmunity [7].
ELS induces microglial priming and alters trajectories of neuroinflammation, creating a vulnerable phenotype wherein subsequent immune challenges provoke exaggerated inflammatory responses [90]. This maladaptive neuroimmune signature is characterized by elevated pro-inflammatory cytokines including IL-6, TNF-α, and CRP, which are consistently observed in individuals with ELS histories [17]. Notably, the relationship between major depressive disorder and inflammation is more pronounced in individuals with childhood adversity compared to those without [17].
Metabolic Programming
ELS induces lasting alterations in energy utilization and metabolic homeostasis. Animal models demonstrate that early-life stress exposure produces metabolic derangements including hyperinsulinemia and altered insulin sensitivity when exposed to high-energy diets later in life [88]. These effects involve programming of both central regulatory mechanisms and peripheral tissues, with alterations in glucocorticoid receptor and 11β-HSD1 expression modulating tissue-specific glucocorticoid availability [88].
Human studies corroborate these findings, showing that adverse early experiences are associated with persisting changes in HPA axis function that predispose to metabolic conditions. Experience of adversity during early life increases the risk of later life obesity and is positively correlated with increased adult BMI in men, independently of mental health condition [88].
Multi-System Pathological Consequences
The maladaptive programming initiated by ELS manifests across multiple physiological systems, creating a diverse spectrum of potential clinical presentations:
Cardiovascular System: Altered autonomic regulation, increased inflammation, and vascular dysfunction [89]
Gastrointestinal System: Gut microbiome alterations, increased intestinal permeability, and gut-brain axis dysregulation [17]
Autoimmune Conditions: HPA axis dysregulation under chronic stress constitutes a critical mechanistic link between psychological stress and autoimmune disease, with evidence associating persistent HPA dysfunction with systemic lupus erythematosus, rheumatoid arthritis, and multiple sclerosis [7]
Table 2: Biomarkers of Stress-Related Pathophysiology Across Systems
| Physiological System | Key Biomarkers | Measurement Approaches | Therapeutic Implications |
|---|---|---|---|
| Neuroendocrine | Cortisol, ACTH, CRF, CAR | Diurnal cortisol, DEX-CRH test, stress reactivity | CRF antagonists, glucocorticoid modulators |
| Immune/Inflammatory | IL-6, TNF-α, CRP, IL-1β | Multiplex cytokine panels, acute phase proteins | Anti-cytokine therapies, anti-inflammatories |
| Metabolic | Insulin, glucose, leptin, adiponectin | HOMA-IR, hyperinsulinemic clamp, adipokine panels | Insulin sensitizers, metabolic modulators |
| Oxidative Stress | ROS, glutathione peroxidase, catalase | Redox assays, oxidative stress panels | Antioxidants, NRF2 activators |
Experimental Models and Methodologies
Preclinical Models of Early Life Stress
Animal models permit controlled environmental manipulation throughout developmental periods and investigation of mechanisms underlying ELS effects:
Maternal Separation: Pups separated from dam for varied periods (15 min to 8 h), affecting HPA axis and behavioral responses in a sex-dependent manner [88].
Maternal Deprivation: Absence of dam for extended periods (e.g., 24 hours), inducing marked elevations in plasma corticosterone and decreases in plasma glucose and leptin [88].
Limited Nesting Material: Chronic stressor for dam and pups through inadequate housing, modeling human childhood neglect with impaired HPA axis activity and behavioral deficits [88].
Prenatal Stress Models: Exposure of pregnant dams to stressors, resulting in offspring with learning deficits, anxious behavior, altered immune function, and cardiovascular changes [91].
Human Research Approaches
Human studies employ diverse methodologies to elucidate ELS effects:
Retrospective Studies: Assessing childhood adversity in adults with established medical conditions, though limited by recall bias [89].
Prospective Longitudinal Studies: Following individuals from childhood to adulthood, establishing temporal precedence [89].
Natural Experiments: Investigating discrete exposures such as famine during pregnancy, providing quasi-experimental evidence [88].
Neuroendocrine Challenge Paradigms: Using pharmacological (e.g., DEX/CRH test) or psychological (e.g., Trier Social Stress Test) probes to assess HPA axis reactivity [89].
Visualization of Key Mechanisms
The following diagrams illustrate core pathways and relationships in the developmental origins of adult disease following early life stress.
Diagram 1: HPA Axis Programming by Early Life Stress
Diagram 2: Neuroimmune Signaling Pathways in Stress Pathophysiology
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating ELS Mechanisms
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| HPA Axis Assessment | Corticosterone/Cortisol ELISA, CRF/ACTH immunoassays, DEX-CRH test reagents | Quantifying neuroendocrine responses, feedback sensitivity | Diurnal variation, pulsatile secretion, stress of handling |
| Epigenetic Analysis | Methylation-specific PCR, ChIP assays, bisulfite sequencing kits | Profiling DNA methylation, histone modifications at candidate genes | Tissue specificity, cell-type resolution requirements |
| Cytokine Profiling | Multiplex cytokine panels, ELISA for IL-6, TNF-α, CRP | Measuring inflammatory biomarkers in serum, CSF, tissue | Dynamic range, cross-reactivity, platform validation |
| Neuroimaging | MRI contrast agents, radioligands for PET, fMRI analysis software | Structural/functional brain mapping, receptor quantification | Spatial resolution, motion artifacts, analytical pipelines |
| Animal Models | C57BL/6 mice, Sprague-Dawley rats, maternal separation apparatus | Controlled ELS exposure, mechanistic interrogation | Species differences, laboratory environment standardization |
Therapeutic Implications and Drug Development
Understanding the developmental programming of disease risk opens novel avenues for therapeutic intervention:
HPA Axis-Targeted Approaches
CRF Receptor Antagonists: Blocking exaggerated CRF signaling in brain regions regulating stress and anxiety [89]
Glucocorticoid Receptor Modulators: Selective receptor modulators to restore feedback sensitivity without complete receptor antagonism [7]
11β-HSD1 Inhibitors: Reducing tissue-specific glucocorticoid regeneration, particularly in metabolic tissues [88]
Anti-Inflammatory Strategies
Cytokine-Targeted Biologics: Monoclonal antibodies against specific pro-inflammatory cytokines (e.g., IL-6, TNF-α) [17]
Neuroimmune Modulators: Drugs targeting microglial activation and neuroinflammation [90]
Timing and Developmental Considerations
The timing of interventions represents a critical consideration in treating ELS-related pathophysiology. Critical period windows may exist for certain interventions, particularly those targeting developmental trajectories. Combined approaches addressing both neuroendocrine dysfunction and inflammatory processes show promise for addressing the multi-system nature of ELS programming [92].
The evidence comprehensively demonstrates that early life stress induces maladaptive programming of the HPA axis and associated systems, creating latent vulnerability for adult disease through neuroendocrine-immune interactions. Future research should focus on:
Multi-omics Approaches: Integrating genomic, epigenomic, transcriptomic, and proteomic data to elucidate comprehensive pathways [7]
Longitudinal Studies: Tracking developmental trajectories from early life to adulthood to identify critical transition points [89]
Resilience Mechanisms: Investigating factors that confer protection against ELS-induced pathophysiology [92]
Translational Biomarkers: Developing validated biomarkers for identifying at-risk individuals and monitoring treatment response [93] [92]
The profound impact of early experiences on lifelong health underscores the imperative for early screening, prevention strategies, and novel therapeutics that target the developmental origins of disease.
The hypothalamic-pituitary-adrenal (HPA) axis represents the body's primary neuroendocrine stress response system, coordinating adaptive physiological reactions to psychological and physical stressors [44]. This complex communication network between the hypothalamus, pituitary gland, and adrenal glands culminates in the production of cortisol, a glucocorticoid hormone with potent immunomodulatory properties [81] [44]. In the context of autoimmune pathogenesis, the HPA axis serves as a critical interface between psychological processes and immunological function, with its dysregulation representing a significant pathway through which chronic stress contributes to loss of self-tolerance and autoimmune disease manifestation [81] [61].
Autoimmune diseases, including rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), and multiple sclerosis (MS), are characterized by a breakdown in immune tolerance to self-antigens, leading to chronic inflammation and tissue damage [81]. While genetic predisposition and environmental factors play established roles in their etiology, growing evidence highlights chronic stress as a significant contributor to immune dysregulation through its impact on the HPA axis [81] [61]. This review synthesizes current understanding of HPA-immune cross-talk in autoimmune pathogenesis, with particular emphasis on mechanistic insights, experimental approaches, and therapeutic implications relevant to RA, lupus, and MS.
HPA Axis Physiology and Stress Response
Core Components and Signaling Cascade
The HPA axis functions through a tightly regulated neuroendocrine cascade [81] [44]:
- Hypothalamus: Paraventricular nucleus (PVN) neurons synthesize and release corticotropin-releasing hormone (CRH) in response to stress signals integrated from limbic structures including the amygdala and prefrontal cortex [81].
- Anterior Pituitary: CRH stimulates corticotrope cells to release adrenocorticotropic hormone (ACTH) into systemic circulation [81] [44].
- Adrenal Cortex: ACTH binds to receptors in the zona fasciculata, stimulating cortisol synthesis and secretion [81].
This system is regulated by a negative feedback mechanism where circulating cortisol inhibits further CRH and ACTH release, restoring homeostasis once the stressor resolves [81] [44].
Circadian Regulation and Immune Interactions
Under physiological conditions, cortisol secretion follows a circadian rhythm with pulsatile release patterns that help synchronize immune responses [81]. Cortisol exerts its effects primarily through intracellular glucocorticoid receptors (GRs), modulating gene transcription by suppressing pro-inflammatory signaling pathways involving transcription factors such as NF-κB and AP-1 [81]. This results in decreased production of pro-inflammatory cytokines (including IL-1β, IL-6, and TNF-α), chemokines, and other immune-activating molecules [81]. Additionally, cortisol inhibits proliferation of T and B lymphocytes and limits leukocyte migration to inflamed tissues, contributing to immune homeostasis [81].
Table 1: Key Hormones and Receptors in HPA-Immune Communication
| Component | Source | Primary Immune Targets | Immunological Effects |
|---|---|---|---|
| Corticotropin-Releasing Hormone (CRH) | Hypothalamus | Immune cells (via CRHR1) | Potentiates inflammatory response; increases vascular permeability |
| Adrenocorticotropic Hormone (ACTH) | Anterior Pituitary | Adrenal cortex, immune cells | Stimulates cortisol production; modulates antibody production |
| Cortisol | Adrenal cortex | Most immune cells | Anti-inflammatory; suppresses cytokine production; inhibits lymphocyte proliferation |
| Glucocorticoid Receptor (GR) | Intracellular receptor | Transcriptional regulator | Mediates cortisol effects; suppresses NF-κB signaling |
| Mineralocorticoid Receptor (MR) | Intracellular receptor | Macrophages, other immune cells | Pro-inflammatory effects when activated |
Chronic Stress-Induced HPA Axis Dysregulation
Mechanisms of Dysregulation
Under conditions of chronic stress, the initially adaptive HPA axis undergoes maladaptive changes that disrupt its regulatory capacity [81] [61]:
- Impaired negative feedback: Prolonged cortisol exposure leads to downregulation of glucocorticoid receptors in key regulatory brain regions (hippocampus, prefrontal cortex), reducing feedback sensitivity [81].
- Glucocorticoid receptor resistance: Diminished GR signaling capacity impairs cortisol-mediated immune suppression, creating a pro-inflammatory state [81].
- Cortisol dysregulation: The system may progress through stages from initial hypercortisolism to eventual adrenal exhaustion or paradoxical hypocortisolism due to adrenal resistance [81] [61].
This dysregulation is further compounded by a shift in cortisol signaling toward mineralocorticoid receptors (MRs) on immune cells, which can promote pro-inflammatory responses through upregulation of cytokines like IL-6 and TNF-α [81].
Impact on Cytokine Networks
Chronic HPA axis dysregulation fundamentally alters the immune environment by disrupting cytokine balance [81]:
- Pro-inflammatory upregulation: Increased production of IL-6, TNF-α, IL-1β, and IL-17
- Anti-inflammatory suppression: Reduced IL-10 and TGF-β activity
- Th1/Th2 imbalance: Shift toward pro-inflammatory T-helper responses
This cytokine environment promotes sustained inflammatory activity, weakens protective immune mechanisms, and shifts the immune response toward autoimmunity [81] [61].
Disease-Specific Mechanisms and Evidence
Rheumatoid Arthritis (RA)
In RA, HPA axis dysfunction contributes to dysregulated inflammation in synovial joints [81]:
- Blunted HPA response: Some RA patients exhibit inadequate cortisol responses to inflammation, permitting unchecked inflammatory activity
- Circadian disruption: Alterations in cortisol rhythm parallel diurnal variations in inflammatory symptoms
- GR resistance: Impaired GR signaling in immune cells reduces cortisol-mediated suppression of synovial inflammation
Systemic Lupus Erythematosus (SLE)
HPA axis alterations in lupus demonstrate complex, sometimes paradoxical features [81]:
- Elevated basal cortisol: Some patients show increased baseline cortisol levels
- Stress-induced exacerbations: Psychological stress frequently precedes disease flares
- Altered stress reactivity: Blunted or exaggerated cortisol responses to stressors depending on disease phase
Multiple Sclerosis (MS)
The HPA axis participates in neuroinflammatory processes central to MS pathogenesis [81]:
- Hyperactive HPA axis: Many MS patients exhibit CRH and cortisol hypersecretion
- Hippocampal involvement: Stress-mediated hippocampal dysfunction may contribute to both mood and cognitive symptoms
- Blood-brain barrier effects: Cortisol dysregulation influences BBB permeability and immune cell trafficking to the CNS
Table 2: HPA Axis Abnormalities in Autoimmune Diseases
| Disease | Basal Cortisol | Stress Response | GR Function | Key Cytokine Alterations |
|---|---|---|---|---|
| Rheumatoid Arthritis | Variable (often blunted) | Frequently attenuated | GR resistance common | ↑ IL-6, TNF-α, IL-1β; ↓ IL-10 |
| Systemic Lupus Erythematosus | Elevated in active disease | Dysregulated (blunted or exaggerated) | Partial resistance | ↑ IL-6, IL-10, IFN-α |
| Multiple Sclerosis | Often elevated | Hyperresponsive in many patients | Altered signaling | ↑ IL-6, TNF-α; Th1/Th17 shift |
Experimental Approaches and Methodologies
Assessing HPA Axis Function in Autoimmunity Research
Neuroendocrine Testing Protocols
Dexamethasone Suppression Test (DST)
- Purpose: Assess GR-mediated negative feedback integrity
- Protocol: Administer dexamethasone (1-2mg orally) at 11PM, measure cortisol at 8AM next morning; impaired suppression indicates GR resistance [81]
- Variants: Dexamethasone-CRH test combines DST with CRH challenge for enhanced sensitivity
Trier Social Stress Test (TSST)
- Purpose: Standardized laboratory stressor to evaluate HPA reactivity
- Protocol: Combination of public speaking and mental arithmetic before panel; measure cortisol at baseline, immediately post-stress, and at 15-30 minute intervals for 1-2 hours
- Application: Used to demonstrate blunted cortisol response in chronic stress and autoimmune conditions
Circadian Rhythm Assessment
- Protocol: Serial salivary or plasma cortisol measurements at multiple timepoints (typically awakening, 30min post-awakening, afternoon, evening)
- Analysis: Curve parameters (awakening response, diurnal slope, total output)
- Findings: Flattened circadian rhythms associated with autoimmune disease activity
Immune-Endocrine Integration Methods
Lymphocyte Glucocorticoid Sensitivity Assay
- Purpose: Quantify GR resistance in immune cells
- Protocol: Isolate PBMCs, stimulate with mitogens (PHA/LPS) ± escalating cortisol doses (10^-9 to 10^-5 M), measure cytokine production (IL-6, TNF-α, IFN-γ) via ELISA
- Calculation: IC₅₀ for cortisol inhibition of cytokine production; higher IC₅₀ indicates GR resistance [81]
Cytokine-Induced HPA Activation
- Protocol: Administer low-dose endotoxin (LPS) or recombinant cytokines (IL-6), measure CRH, ACTH, and cortisol response
- Application: Demonstrates bidirectional communication between immune activation and HPA axis
In vivo Stress Models with Immune Challenge
- Protocol: Apply chronic stress paradigm (chronic mild stress, social defeat) in animal models, followed by immune challenge (autoantigen immunization, adjuvant-induced arthritis)
- Endpoint measures: Disease severity, autoantibody production, cytokine profiles, HPA hormone levels
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating HPA-Immune Interactions
| Reagent/Category | Specific Examples | Research Applications | Technical Notes |
|---|---|---|---|
| GR Antagonists | Mifepristone (RU-486) | Determining GR-specific effects in experimental systems | Validates GR-dependent mechanisms; use carefully in vivo |
| CRH Receptor Antagonists | Antalarmin, NBI-27914 | Blocking CRH signaling to dissect stress-immune pathways | Central vs peripheral administration yields different effects |
| Corticosterone/Cortisol Assays | ELISA, RIA, LC-MS/MS | Quantifying hormone levels in plasma, saliva, tissue | Salivary free cortisol reflects biologically active fraction |
| GR Signaling Reporters | GRE-luciferase constructs, GR-GFP fusion | Visualizing and quantifying GR activation and trafficking | Cell-type specific expression reveals tissue-specific regulation |
| Cytokine Measurement | Multiplex bead arrays, ELISA, ELISpot | Profiling inflammatory mediators | Combine with hormone measures for integrated analysis |
| Animal Models of Chronic Stress | Chronic mild stress, social defeat, restraint stress | Modeling psychogenic stress effects on autoimmunity | Strain differences significant; validate disease endpoints |
Therapeutic Implications and Future Directions
Current Therapeutic Approaches
Conventional treatments for autoimmune diseases primarily target downstream inflammatory processes, but understanding HPA-immune cross-talk opens opportunities for novel interventions [81]:
- Stress management integration: Cognitive-behavioral therapy, mindfulness, and relaxation techniques as adjunctive treatments
- Circadian rhythm optimization: Timing of medications to align with endogenous cortisol rhythms
- Combination neuroendocrine-immunomodulatory approaches: Coordinated targeting of both systems
Emerging Therapeutic Strategies
Recent research has revealed several promising approaches that target HPA-immune interactions [94]:
- Precision immunotherapies: Engineering T-cell engagers that selectively target autoreactive B cells while sparing protective immunity [94]
- mRNA-based approaches: Instructing immune regulatory cells to suppress pathogenic T cells and promote tolerance [94]
- Microbiome-targeted interventions: Probiotics, prebiotics, and dietary modifications to modulate HPA axis function through the gut-brain axis [15] [95]
- Vagus nerve stimulation: Leveraging the cholinergic anti-inflammatory pathway to suppress inflammation [96]
Visualizing HPA-Immune Signaling Pathways
Core HPA-Immune Signaling Pathway
Chronic Stress-Induced HPA Dysregulation in Autoimmunity
The intricate cross-talk between the HPA axis and immune system represents a fundamental mechanistic pathway through which chronic stress contributes to autoimmune pathogenesis. Dysregulation of this bidirectional communication system—characterized by glucocorticoid resistance, cortisol rhythm disruption, and maladaptive cytokine signaling—creates a permissive environment for loss of self-tolerance and sustained inflammation in diseases including rheumatoid arthritis, lupus, and multiple sclerosis. Understanding these neuroendocrine-immune interactions not only provides insight into disease mechanisms but also reveals novel therapeutic opportunities that simultaneously target both systems. Future research should focus on longitudinal studies mapping temporal relationships between stress, HPA function, and autoimmune progression, alongside development of personalized medicine approaches that account for individual variations in stress responsiveness and neuroimmune function.
The gut-brain axis represents a complex, bidirectional communication network that intricately links the gastrointestinal tract with the central nervous system. Within this framework, the hypothalamic-pituitary-adrenal (HPA) axis serves as the body's primary neuroendocrine stress response system, and emerging research has revealed its profound susceptibility to modulation by gut microbiota. The microbial ecosystem inhabiting the mammalian gastrointestinal tract engages in extensive cross-talk with the HPA axis through multiple signaling pathways, including neural connections (vagus nerve), immune mediators (cytokines), microbial metabolites (short-chain fatty acids), and neuroendocrine factors (cortisol) [28] [30] [97].
Disruption of this delicate communication system has significant clinical implications. Disorders of the microbiota-gut-brain axis are frequently associated with HPA axis dysregulation, observed in conditions such as major depressive disorder, anxiety disorders, and irritable bowel syndrome [28] [97]. Preclinical models demonstrate that germ-free mice exhibit altered stress responses and neurodevelopment, which can be normalized through microbial colonization, highlighting the essential role of microbiota in HPA axis programming [28] [30]. This interaction forms the scientific foundation for microbiota-targeted interventions aimed at restoring neuroendocrine homeostasis in stress-related pathologies.
Mechanisms of Gut Microbiota-HPA Axis Communication
Key Signaling Pathways
The communication between gut microbiota and the HPA axis occurs through several integrated biological pathways, each contributing to the overall regulation of stress responses and neurological function.
Neural Pathways: The vagus nerve serves as a direct neural connection between the gut and brain, transmitting microbial signals that influence emotional regulation and stress responses [97]. Research indicates that vagus nerve stimulation produces anxiolytic effects through noradrenergic pathways and modulates neurotransmitter systems, including α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPAR)-mediated excitatory neurotransmission in the central amygdala [97].
Endocrine Pathways: The HPA axis itself functions as a primary endocrine pathway. Gut microbiota composition directly influences the secretion of corticotropin-releasing hormone (CRH) from the hypothalamic paraventricular nucleus, which prompts anterior pituitary secretion of adrenocorticotropic hormone (ACTH), ultimately stimulating glucocorticoid (cortisol) production from the adrenal cortex [97] [27]. Appropriate concentrations of cortisol are essential for normal neurodevelopment, cognitive processes, and feedback regulation of the HPA axis [27].
Immune Pathways: The gut-immune-brain axis represents a critical communication route where microbial components such as lipopolysaccharides (LPS) and peptidoglycans interact with pattern recognition receptors including Toll-like receptors (TLRs) [28] [30]. This interaction modulates the production of pro-inflammatory cytokines (e.g., IL-6, IL-1β, TNF-α) that can activate the HPA axis and influence blood-brain barrier permeability [28] [30] [97].
Metabolic Pathways: Gut microbiota produce various neuroactive metabolites, including short-chain fatty acids (SCFAs) such as acetate, butyrate, and propionate through fermentation of dietary fiber [98] [30]. These metabolites function as histone deacetylase inhibitors and activate G protein-coupled receptors (GPR41, GPR43, GPR109A), influencing neuroinflammation, neurotransmitter synthesis, and HPA axis reactivity [98] [30].
The following diagram illustrates the complex bidirectional communication within the gut-immune-brain axis and its regulation of the HPA axis:
Experimental Evidence from Preclinical Models
Preclinical models have been instrumental in elucidating the causal relationships between gut microbiota and HPA axis function. Germ-free mice demonstrate heightened HPA responses to stress, with significantly increased ACTH and corticosterone levels following restraint stress compared to conventionally colonized controls [28]. This hyperactive stress response is normalized following colonization with specific pathogen-free microbiota, but only during early life development, indicating a critical window for microbial programming of the HPA axis [28].
Early life stress models further demonstrate the persistent programming effects on the HPA axis. Maternal separation stress in rodents leads to long-term hyperreactivity of the HPA axis, increased CRF signaling, and impaired glucocorticoid receptor-mediated negative feedback [28]. These neuroendocrine changes are accompanied by altered gut microbiota composition and increased intestinal permeability, suggesting interconnected pathophysiology [28]. Additionally, neonatal exposure to bacterial components such as lipopolysaccharide produces enduring changes in HPA axis reactivity, cerebral glucocorticoid receptor density, and CRF expression that persist into adulthood [28].
The causal role of specific microbiota in transferring behavioral phenotypes has been demonstrated through fecal microbiota transplantation studies. Transplantation of microbiota from patients with major depressive disorder to germ-free rodents induces depression-like behaviors and alters tryptophan metabolism in recipient animals [28] [99]. Similarly, transplantation of microbiota from social anxiety disorder patients to mice heightens sensitivity to social fear and alters immune and oxytocin systems [99].
Gut Microbiota Interventions: Mechanisms and Methodologies
Probiotics and Psychobiotics
Probiotics are defined as live microorganisms that, when administered in adequate amounts, confer health benefits on the host [98]. When specifically targeted toward mental health applications, these are often termed "psychobiotics" and represent a promising intervention for modulating the gut-brain axis.
Table 1: Clinically Studied Probiotic Strains and Their Neuroactive Effects
| Strain | Dosage (CFU/day) | Experimental Model | Observed Effects on HPA Axis/Behavior |
|---|---|---|---|
| Lactobacillus and Bifidobacterium mixtures | 10^9-10^10 | Human clinical trials (depression) | Significant decrease in Beck Depression Inventory scores; reduced depressive symptoms as add-on therapy [98] [99] |
| Lactobacillus rhamnosus JB-1 | 10^9 | Rodent stress models | Reduced stress-induced corticosterone; anxiolytic effects dependent on vagus nerve [28] |
| Multistrain probiotics | 10^9-10^10 | Human pilot trial (depression) | Greater reductions in depression/anxiety symptoms vs. placebo as adjunct to antidepressants [99] |
| Bacillus species | Not specified | Human follow-up study | Increased abundance correlated with reduced anxiety symptoms [99] |
The proposed mechanisms of probiotic action on the HPA axis include:
- Reduction of pro-inflammatory cytokines and modulation of systemic inflammation [98]
- Enhancement of tight junction proteins in the gut epithelium, reducing intestinal permeability and subsequent immune activation [28]
- Production of neuroactive metabolites including GABA, serotonin precursors, and SCFAs [97]
- Competitive exclusion of pathobionts that may produce neurotoxic metabolites [98]
- Modulation of vagal afferent signaling to CNS regions involved in stress and emotion regulation [97]
Prebiotics
Prebiotics are defined as selectively fermented ingredients that result in specific changes in the composition and/or activity of the gastrointestinal microbiota, thereby conferring benefits upon host health [98]. They primarily consist of non-digestible carbohydrates that resist gastric acidity and hydrolysis by mammalian enzymes, reaching the colon intact to serve as substrates for beneficial bacteria.
Table 2: Common Prebiotics and Their Effects on Gut-Brain Axis
| Prebiotic Type | Effective Daily Dose | Microbial Targets | Documented Effects on Neuroendocrine Function |
|---|---|---|---|
| Fructooligosaccharides (FOS) | 10 g | Bifidobacterium, Lactobacillus | Improves stress resilience, modulates HPA axis reactivity, increases SCFA production [98] |
| Galactooligosaccharides (GOS) | 7 g | Bifidobacterium, Lactobacillus | Reduces waking cortisol response, decreases attentional vigilance to negative information [98] |
| Polydextrose | 2-7.5 g | Bifidobacterium | Improves cognitive performance, modulates inflammatory markers [98] |
| Resistant Starch | 2.5-5 g | Bifidobacterium, Roseburia | Enhances gut barrier function, reduces systemic inflammation [98] |
| Inulin | 1-6 g | Bifidobacterium | Improves memory function, reduces neuroinflammation [98] |
The molecular mechanisms whereby prebiotics influence the HPA axis include:
- Increased production of SCFAs through bacterial fermentation, which can modulate peripheral and central inflammatory responses [98] [30]
- Enhanced production of gut hormones (e.g., GLP-1, PYY) that influence brain function and HPA axis activity [98]
- Reduction of bacterial translocation through enhanced gut barrier function, decreasing systemic immune activation [28]
- Alteration of bile acid metabolism, which can function as signaling molecules in the brain and periphery [30]
Fecal Microbiota Transplantation
Fecal microbiota transplantation involves the transfer of processed stool material from a healthy donor into the gastrointestinal tract of a recipient, with the goal of restoring a healthy microbial ecosystem. This intervention represents the most comprehensive approach to microbiota modification, transferring an entire community of microorganisms rather than selected strains.
Table 3: FMT Protocols and Outcomes in Preclinical and Clinical Studies
| Condition Model | FMT Protocol | Effects on HPA Axis/Neuroendocrine Function | Key Microbial Changes |
|---|---|---|---|
| Experimental Autoimmune Encephalomyelitis | FMT from healthy donors | Improved neurological function; reduced serum cortisol and IL-17; effects dependent on intact HPA axis [100] | Increased abundance of beneficial flora; restored intestinal homeostasis [100] |
| Depression (Human) | FMT from healthy donors to patients with treatment-resistant depression | Transformative improvement in depressive symptoms within one week; enabled antidepressant efficacy [99] | Not fully characterized; presumed restoration of normative microbial diversity [99] |
| Depression (Rodent) | FMT from depressed patients to germ-free mice | Induced anhedonia and anxiety-like behaviors; altered tryptophan metabolism [28] [99] | Transfer of depression-associated microbial profile [28] |
| Irritable Bowel Syndrome with Anxiety | FMT from IBS patients with anxiety to germ-free mice | Induced anxiety-like behavior; enhanced expression of colonic glucocorticoid receptor pathway genes [28] | Transfer of IBS-associated microbiota with immune activation [28] |
The following diagram illustrates a standardized experimental workflow for evaluating FMT in preclinical models of HPA axis dysfunction:
Research Reagent Solutions for Gut-Brain Axis Investigations
Table 4: Essential Research Reagents for Investigating Microbiota-HPA Axis Interactions
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Probiotic Strains | Lactobacillus rhamnosus JB-1, Bifidobacterium longum 1714, Lactobacillus helveticus R0052 | Mechanistic studies of specific strains on HPA axis function in preclinical models | Viability verification, colonization stability, administration vehicle compatibility [98] |
| Prebiotic Compounds | FOS, GOS, Inulin, Resistant Starch, Polydextrose | Investigation of microbial metabolite production and HPA axis effects | Purity assessment, dose-response characterization, fermentation kinetics [98] |
| Gnotobiotic Models | Germ-free mice, Humanized microbiota mice | Causal studies of microbial influence on HPA axis development and function | Strict containment protocols, careful microbial reconstitution designs [28] [30] |
| Molecular Analysis Tools | 16S rRNA sequencing, Metagenomics, Metabolomics (LC-MS/MS) | Comprehensive assessment of microbial community structure and function | Sample preservation methods, DNA/RNA extraction efficiency, bioinformatic pipeline standardization [101] |
| HPA Axis Assessment | Corticosterone/Cortisol ELISA, CRF/ACTH immunoassays, Glucocorticoid receptor antagonists | Quantification of neuroendocrine stress response parameters | Diurnal rhythm considerations, sampling frequency, stress-free collection methods [28] [27] |
| Barrier Function Assays | FITC-dextran permeability, Tight junction protein immunostaining (ZO-1, occludin), LPS measurements | Evaluation of gut and blood-brain barrier integrity | Tissue processing standardization, endothelial cell isolation protocols [28] [30] |
The burgeoning field of gut microbiota interventions represents a paradigm shift in our understanding of neuroendocrine regulation and stress pathophysiology. The evidence summarized in this review demonstrates that probiotics, prebiotics, and fecal microbiota transplantation offer promising avenues for modulating HPA axis function through targeted manipulation of the gut-brain axis. The mechanistic insights gleaned from preclinical models reveal complex, multidirectional communication pathways involving neural, endocrine, immune, and metabolic signaling systems.
While substantial progress has been made in elucidating the fundamental principles of microbiota-HPA axis interactions, several challenges remain before these interventions can be widely translated into clinical practice. Future research priorities include: standardization of intervention protocols across studies, identification of predictive biomarkers for treatment response, understanding of critical windows for intervention across the lifespan, and development of personalized approaches based on individual microbial and neuroendocrine profiles. Large-scale human trials with parallel mechanistic analyses are urgently needed to translate promising preclinical findings into effective, evidence-based therapies for stress-related disorders.
The integration of microbiota-targeted interventions with conventional pharmacological approaches may ultimately yield novel treatment strategies for the numerous psychiatric, neurological, and gastrointestinal disorders characterized by HPA axis dysregulation. As our understanding of the gut-immune-brain axis continues to evolve, so too will opportunities to develop innovative therapeutic interventions that leverage this fundamental physiological connection.
Cross-System Analysis and Translational Validation of HPA Interactions
The hypothalamic-pituitary-adrenal (HPA) axis and hypothalamic-pituitary-gonadal (HPG) axis represent two primary neuroendocrine systems that integrate neural and endocrine signaling to regulate fundamental physiological processes. The HPA axis serves as the body's central stress response system, while the HPG axis governs reproductive functions and steroid hormone production. Historically studied in isolation, emerging evidence reveals extensive bidirectional crosstalk between these systems that critically modulates complex behaviors, particularly aggression [62] [102]. This review synthesizes current understanding of HPA-HPG interactions in stress-induced aggression, providing researchers and drug development professionals with a comprehensive technical framework for investigating these complex neuroendocrine pathways.
Understanding the mechanistic basis of HPA-HPG interactions requires examining both axes at molecular, cellular, and circuit levels. The following sections detail the physiology and regulation of each axis independently before exploring their integrative neurobiology in aggression models. Experimental methodologies for quantifying these interactions and identifying novel therapeutic targets are also presented.
The Hypothalamic-Pituitary-Adrenal (HPA) Axis: Physiology and Regulation
Anatomical and Functional Organization
The HPA axis constitutes a coordinated neuroendocrine circuit comprising the hypothalamus, pituitary gland, and adrenal glands [44]. This system maintains homeostasis through a cascade of hormonally-driven events initiated in response to physiological or psychological stressors [62]. The paraventricular nucleus (PVN) of the hypothalamus serves as the central regulatory center, housing neurosecretory parvocellular neurons that synthesize and secrete key regulatory factors [3].
Critical transcription factors governing PVN development and function include:
- Brn-2: A POU-homeodomain protein essential for terminal differentiation of CRH parvocellular neurons and OT/AVP magnocellular neurons [3]
- Otp: A homeobox gene regulating differentiation and maturation of neurosecretory PVN neurons expressing TRH, AVP, and OT [3]
- Sim1: A transcription factor regulating AVP, TRH, CRH, OT, and somatostatin expression; Sim1 knock-out mice show severe loss of these neurons [3]
Neuroendocrine Signaling Cascade
The HPA axis activation follows a sequential hormonal cascade:
- Corticotropin-releasing hormone (CRH) release from parvocellular PVN neurons into the hypophyseal portal system [62]
- Adrenocorticotropic hormone (ACTH) secretion from anterior pituitary corticotropes in response to CRH [44]
- Glucocorticoid (cortisol in humans, corticosterone in rodents) production from adrenal cortex stimulated by ACTH [62]
CRH action is modulated by arginine vasopressin (AVP), co-released from PVN neurons, which synergistically enhances ACTH secretion through V1b receptors on pituitary corticotropes [62]. The CRH type 1 receptor (CRF1) is predominantly expressed in the anterior pituitary and limbic regions, while CRF2 is primarily found in peripheral tissues and subcortical structures [62]. A binding protein (CRF-BP) regulates CRH bioavailability, with 40-60% of CRF bound to CRF-BP under normal conditions [62].
Table 1: Core Components of the HPA Axis
| Component | Key Structures/Cells | Secreted Factors | Primary Functions |
|---|---|---|---|
| Hypothalamus | Paraventricular Nucleus (PVN) parvocellular neurons | CRH, AVP | Integrate stress signals; initiate neuroendocrine cascade |
| Anterior Pituitary | Corticotrope cells | ACTH | Stimulate adrenal glucocorticoid production |
| Adrenal Glands | Adrenal cortex | Cortisol (corticosterone) | Mediate systemic stress responses; regulate metabolism, immunity |
Regulatory Mechanisms and Feedback Loops
The HPA axis is regulated through sophisticated feedback mechanisms that terminate stress responses and maintain homeostasis. Glucocorticoids exert negative feedback at multiple levels:
- Fast feedback: Via membrane-associated receptors in the PVN and pituitary
- Delayed feedback: Through genomic actions via glucocorticoid receptors (GR) and mineralocorticoid receptors (MR) [62]
Chronic stress can induce HPA axis dysregulation, leading to altered cortisol levels and impaired feedback sensitivity [62] [102]. This dysregulation manifests as either hyperactive or hypoactive HPA axis function, contributing to pathological states including mood disorders, metabolic syndrome, and aggression-related conditions [44].
The Hypothalamic-Pituitary-Gonadal (HPG) Axis: Physiology and Androgen Signaling
Functional Organization and Regulation
The HPG axis regulates reproductive function through a coordinated hierarchy of hormonal signaling. Gonadotropin-releasing hormone (GnRH) neurons in the preoptic area and hypothalamus initiate the cascade by pulsatile GnRH release into the hypophyseal portal system. GnRH stimulates anterior pituitary gonadotropes to secrete luteinizing hormone (LH) and follicle-stimulating hormone (FSH), which subsequently regulate gonadal steroidogenesis and gametogenesis [102].
The primary androgen, testosterone, exerts organizational effects during development and activational effects in adulthood. Testosterone and its metabolite, dihydrotestosterone (DHT), bind androgen receptors (AR) widely distributed throughout the brain's neural circuitry, particularly in regions implicated in aggressive behavior including the medial amygdala, ventromedial hypothalamus, and prefrontal cortex [62] [102].
Androgen Receptor Signaling and Neural Circuitry
Androgen receptors function as ligand-activated transcription factors that modulate gene expression in target tissues. In the brain, AR activation influences neuronal excitability, synaptic plasticity, and circuit function through both genomic and non-genomic mechanisms. The neural circuitry of aggression involves a distributed network including:
- Medial amygdala: Processes socially relevant stimuli
- Ventromedial hypothalamus: Integrates aggressive signals
- Prefrontal cortex: Provides top-down inhibitory control
- Periaqueductal gray: Executes aggressive responses [62]
Animal and human studies consistently demonstrate positive associations between testosterone levels and aggression, particularly in contexts of social provocation or competition [62] [102]. Androgen action in these circuits modulates aggressive behavior by altering neuronal responsiveness to provocative stimuli.
Table 2: Experimental Evidence for HPA-HPG Interactions in Aggression
| Study Type | Experimental Model | Key Findings | Methodological Approach |
|---|---|---|---|
| Animal Studies | Rodent resident-intruder test | Chronic stress alters cortisol and increases offensive aggression | Hormone measurement, behavioral scoring |
| Human Studies | Psychosocial stress tests | Cortisol and testosterone responses predict aggressive behavior | Trier Social Stress Test, Point Subtraction Aggression Paradigm |
| Clinical Correlational | Aggression-related disorders | HPA dysregulation and altered testosterone profiles | Hormonal profiling, neuropsychological assessment |
HPA-HPG Cross-talk: Molecular Mechanisms and Behavioral Integration
Neuroendocrine Interactions at Multiple Levels
The HPA and HPG axes exhibit complex bidirectional interactions that occur at multiple regulatory levels:
Central nervous system cross-talk:
- CRH and glucocorticoids suppress GnRH pulsatility [62]
- Gonadal steroids modulate CRH gene expression and HPA axis activity [102] [3]
Peripheral interactions:
- Glucocorticoids inhibit gonadal steroidogenesis directly at the testicular and ovarian levels [62]
- Testosterone and estrogen influence adrenal sensitivity to ACTH [102]
Shared regulatory mechanisms:
- Common transcription factors and co-regulators
- Overlapping enzyme systems for steroid hormone metabolism
- Convergent signaling pathways in limbic circuits [62] [102]
Stress-Induced Modulation of Aggressive Behavior
Stress experiences differentially modulate aggressive behavior depending on timing, duration, and context. Acute stress typically potentiates aggression through rapid glucocorticoid and catecholamine actions, while chronic stress often leads to either escalated or diminished aggression depending on the resulting HPA/HPG adaptation [62].
The dual-hormone hypothesis proposes that testosterone and cortisol interact to predict aggression, with testosterone positively correlating with aggression primarily when cortisol levels are low [62] [102]. This interaction reflects the competing demands of stress response and reproductive strategies.
Chronic stress can induce HPA axis dysregulation, leading to altered cortisol levels and potentially contributing to aggressive behavior [62] [102]. The HPG axis, particularly the androgen hormone testosterone, is also closely linked to aggression [62] [102].
Experimental Methodologies for Investigating HPA-HPG Interactions
Hormonal Assessment Protocols
Sample Collection and Processing:
- Blood samples collected between 7:30-8:30 a.m. after overnight fast to control for diurnal variation [103]
- Use EDTA-containing tubes, immediate centrifugation at 2,000×g for 10 min at 4°C [103]
- Secondary centrifugation at 13,000×g for 10 min at 4°C to remove cellular debris [103]
- Plasma storage at -80°C until analysis to preserve hormone integrity [103]
Hormonal Assays:
- Cortisol: Measured by commercial radioimmunoassay or ELISA [103]
- ACTH: Quantified using immunoradiometric or chemiluminescent assays
- Testosterone: Assessed via liquid chromatography-mass spectrometry (gold standard) or immunoassay
- CRH and AVP: Measured in hypophyseal portal blood or cerebrospinal fluid in animal models [62]
Stress Hormone Response Assessment:
- Trier Social Stress Test for standardized psychosocial stress response [103]
- CRH stimulation test to assess pituitary ACTH reserve
- Dexamethasone suppression test to evaluate HPA negative feedback integrity
Molecular and Genetic Approaches
Circulating miRNA Profiling:
- Total RNA extraction from plasma using Trizol LS protocol [103]
- miRNA expression analysis via quantitative RT-PCR or next-generation sequencing
- Identification of stress-responsive miRNAs (let-7b, miR-142, miR-144, miR-29a) associated with HPA/HPG function [103]
Gene Expression Analysis:
- In situ hybridization for neuropeptide mRNA localization in brain tissue
- Quantitative PCR of microdissected brain regions
- Single-cell RNA sequencing of hypothalamic nuclei
Epigenetic Modifications:
- Chromatin immunoprecipitation for transcription factor binding sites
- DNA methylation analysis of hormone receptor gene promoters
- Histone modification mapping in stress-responsive genes
Behavioral Paradigms for Aggression Assessment
Animal Models:
- Resident-intruder test: Measures offensive aggression in territorial males [62]
- Maternal aggression test: Assesses protective aggression in lactating females [62]
- Social isolation: Induces hyper-aggressiveness in rodents
- Vicarious social defeat: Models psychosocial stress effects on aggression
Human Laboratory Models:
- Point Subtraction Aggression Paradigm: Measures aggressive responses to provocation
- Taylor Aggression Paradigm: Assesss retaliatory behavior
- Competitive Reaction Time Task: Quantifies aggression as noise blast administration
Table 3: Research Reagent Solutions for HPA-HPG Investigation
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Hormone Assay Kits | Cortisol RIA, ELISA Testosterone LC-MS/MS | Quantitative hormone measurement | Cross-reactivity assessment; validation against gold standard methods |
| CRH Receptor Ligands | CRF1 antagonists (Antalarmin) CRF2 agonists | Receptor-specific pathway manipulation | Blood-brain barrier penetration; receptor selectivity |
| Androgen Receptor Modulators | Flutamide (antagonist) Dihydrotestosterone (agonist) | Androgen signaling manipulation | Tissue-specific distribution; metabolite activity |
| miRNA Analysis | Trizol LS, qRT-PCR primers for let-7b, miR-142, miR-144, miR-29a | Stress-responsive miRNA profiling | RNA stability; normalization controls [103] |
| Steroidogenic Enzyme Inhibitors | Metyrapone (CYP11B1 inhibitor) Ketoconazole (broad cytochrome P450 inhibitor) | HPA axis manipulation; steroid synthesis blockade | Specificity; compensatory mechanisms |
Neurobiological Substrates of HPA-HPG Interactions in Aggression
Neural Circuitry of Aggression
Aggressive behavior is regulated by a conserved neural network that integrates social information, internal state, and environmental context. Key nodes include:
Prefrontal cortex (PFC): Provides top-down inhibitory control over aggressive impulses. Stress-induced glucocorticoids impair PFC function, reducing inhibitory control and facilitating aggression [62].
Amygdala: Processes threat-related stimuli and initiates aggressive responses. Glucocorticoids and androgens synergistically enhance amygdala reactivity to provocative stimuli [62].
Hypothalamus: Serves as a central executive for aggressive behavior. The ventromedial hypothalamus (VMH) and medial hypothalamus integrate hormonal and neural signals to coordinate aggressive displays [62].
Midbrain periaqueductal gray (PAG): Translates aggressive signals into coordinated somatic and autonomic responses [62].
Neuropeptide and Neurotransmitter Systems
Multiple neurotransmitter systems mediate HPA-HPG interactions in aggression:
Vasopressin: Potentiates aggression through actions in the medial amygdala and anterior hypothalamus. Androgens upregulate vasopressin V1a receptor expression [62].
Serotonin: Generally inhibits aggression via projections from raphe nuclei to prefrontal cortex, amygdala, and hypothalamus. Serotonin deficiency is associated with increased impulsivity and aggression [62].
Dopamine: Modulates aggression reward aspects through mesolimbic pathways. Dopamine signaling in nucleus accumbens may reinforce aggressive behavior under certain conditions [62].
The intricate bidirectional communication between the HPA and HPG axes represents a fundamental mechanism coordinating stress adaptation and reproductive strategies. Dysregulation of these interactions contributes significantly to pathological aggression across multiple species. Future research should prioritize:
- Circuit-level mechanisms: Defining precise neural pathways through which stress and gonadal hormones converge to modulate aggression
- Developmental programming: Investigating how early life stress permanently organizes HPA-HPG interactions and aggression susceptibility
- Sex differences: Systematic examination of how HPA-HPG interactions differentially regulate aggression in males and females
- Therapeutic targeting: Developing pharmacological interventions that specifically target HPA-HPG cross-talk for aggression-related disorders
Advanced techniques including in vivo calcium imaging, optogenetics, chemogenetics, and circuit-level transcriptomics will enable unprecedented resolution of these neuroendocrine interactions. Integration across molecular, cellular, circuit, and behavioral levels will provide a comprehensive framework for understanding and treating pathological aggression through targeted modulation of HPA-HPG axis interactions.
The hypothalamic-pituitary-adrenal (HPA) axis, a critical neuroendocrine circuit, governs the body's physiological response to internal and external stressors. A fundamental characteristic of this system is its sexual dimorphism [104]. In adult rodents, the acute stress-induced activation of the HPA axis is markedly greater in females than in males, a pattern that has significant implications for sex-biased vulnerability to stress-related pathologies [104]. This sex difference arises from the complex interplay of genetic and hormonal factors, primarily mediated by the organizational and activational effects of gonadal steroids [104] [105]. Organizational effects refer to the permanent, developmental actions of hormones during critical prenatal and neonatal periods that shape brain circuitry. In contrast, activational effects are transient and occur in adulthood, modulating the function of pre-established circuits in response to circulating hormone levels [105]. This whitepaper synthesizes current evidence on how these effects govern sex differences in HPA axis responsiveness, providing a technical guide for researchers and drug development professionals working in stress neurobiology.
HPA Axis Physiology and Sexual Dimorphism
Core Circuitry and Regulation
The HPA axis is a cascade of neuroendocrine signaling events. It begins with the synthesis and release of corticotropin-releasing hormone (CRH) and arginine vasopressin (AVP) from parvocellular neurons of the paraventricular nucleus (PVN) of the hypothalamus [104] [62]. These neuropeptides are secreted into the hypothalamic-pituitary portal vasculature and stimulate the anterior pituitary to release adrenocorticotropic hormone (ACTH) into systemic circulation [104]. ACTH, in turn, acts on the adrenal cortex to stimulate the synthesis and secretion of glucocorticoids—corticosterone in rodents and cortisol in humans [104]. Glucocorticoids exert widespread effects on energy mobilization, cognition, and immune function, while also acting on the brain, pituitary, and hypothalamus to inhibit further HPA activation via negative feedback mechanisms primarily mediated by glucocorticoid receptors (GR) and mineralocorticoid receptors (MR) [104].
Established Sex Differences in HPA Axis Output
Robust sex differences are observed at multiple levels of the HPA axis. Following an acute stressor, adult female rodents exhibit significantly greater and more prolonged elevations of both ACTH and CORT compared to males [104]. This is associated with:
- Greater neuronal activation (e.g., c-Fos expression) in the PVN following various stressors [104].
- Higher expression of HPA-related genes, including CRH, AVP mRNA in the PVN, and POMC (the ACTH precursor) mRNA in the anterior pituitary [104].
- Delayed return to baseline hormone levels, indicating differences in the efficiency of negative feedback inhibition [104].
Table 1: Documented Sex Differences in Rodent HPA Axis Parameters
| Parameter | Observation in Females vs. Males | Key References |
|---|---|---|
| ACTH & CORT Secretion | Greater peak amplitude and delayed recovery after acute stress. | [104] |
| PVN Activation | Increased c-Fos immunoreactivity and immediate-early gene expression. | [104] |
| Gene Expression | Higher basal and stress-induced CRH and AVP mRNA in PVN. | [104] |
| Negative Feedback | Less efficient glucocorticoid-mediated feedback. | [104] |
Organizational vs. Activational Effects of Gonadal Hormones
The prevailing model posits that sex differences in HPA function are determined by both the early-life organizational actions of gonadal hormones and their later-life activational effects [104] [105].
Organizational Effects
Organizational effects program the brain during a critical perinatal period, establishing lifelong sex differences in neural structure and function. In rodents, the presence of testicular androgens and their estrogenic metabolites in males during this period masculinizes and defeminizes the HPA axis stress response circuitry, leading to a attenuated response in adulthood [104] [105]. The absence of this androgen surge in females results in a brain that supports a more robust HPA response to stress. These effects are considered permanent and are not reversed by gonadectomy in adulthood [105].
Activational Effects
Activational effects are transient and depend on the circulating levels of gonadal hormones in adulthood. These effects modulate the sensitivity and magnitude of the stress response on a pre-established neural substrate organized during development.
- Estradiol (E₂): Generally has a potentiating effect on the HPA axis. In female rodents and in estrogen-treated castrated males, E₂ enhances the ACTH and CORT response to stressors like alcohol and restraint [105]. It is associated with increased CRH and AVP mRNA expression in the PVN [105].
- Testosterone (T): Generally has an inhibitory effect on the HPA axis. Castration of adult male rats increases HPA responsiveness, which is normalized by testosterone replacement [105] [106]. This inhibition can be mediated directly via androgen receptors (AR) or indirectly after aromatization to estradiol, influencing feedback and hypothalamic neuropeptide systems [106].
Table 2: Summary of Gonadal Hormone Effects on the HPA Axis
| Hormone | Effect Type | Impact on HPA Axis Responsiveness | Proposed Mechanisms |
|---|---|---|---|
| Estradiol | Activational | Potentiates | Increases CRH/AVP mRNA; reduces feedback sensitivity. |
| Testosterone | Activational | Inhibits | AR-mediated inhibition of HPA activity; modulation of CRH systems. |
| Perinatal Androgens | Organizational | Attenuates (in males) | Permanently organizes neural circuits for a blunted adult response. |
The following diagram illustrates the interplay of organizational and activational effects in shaping the adult HPA axis phenotype in males and females.
Molecular Mechanisms and Neural Substrates
Hypothalamic Neuropeptides
Gonadal steroids exert significant influence over the expression and secretion of key HPA axis secretagogues.
- CRH and AVP: Estradiol upregulates CRH and AVP mRNA expression in the PVN [105]. Androgens, conversely, inhibit the stress-induced increase in hypothalamic CRH [105] [106]. The ratio and co-expression of these peptides, which is sexually dimorphic, can determine the magnitude of the ACTH response.
- Oxytocin and Others: Androgens and estrogens also modulate other neuropeptide systems like oxytocin, dopamine, and serotonin within hypothalamic and limbic circuits, indirectly fine-tuning HPA axis output [106].
Negative Feedback and Glucocorticoid Signaling
The delayed return of glucocorticoids to baseline in females suggests less efficient negative feedback. This may be due to sex differences in:
- Glucocorticoid Receptor (GR) and Mineralocorticoid Receptor (MR) expression in key feedback sites like the hippocampus, prefrontal cortex, and PVN [104].
- GR translocation and downstream gene transcription events that terminate the stress response [104].
Limbic Regulation
Sex differences in the HPA axis are also governed by upstream limbic brain regions.
- The amygdala (particularly the medial and central nuclei), which provides excitatory drive to the PVN, shows sex-dependent function and steroid hormone receptor expression [104].
- The bed nucleus of the stria terminalis (BNST), a key relay between the amygdala and PVN, is highly sexually dimorphic and rich in steroid receptors, influencing HPA inhibition [104].
- The hippocampus and prefrontal cortex, which provide inhibitory input to the PVN, also exhibit structural and functional sex differences that contribute to differential feedback and regulation of the psychological stress response [104].
The following diagram summarizes the key neural circuits and molecular sites where gonadal hormones act to create sex differences in HPA axis responsiveness.
Experimental Paradigms and Key Methodologies
Research into organizational and activational effects relies on specific, well-established experimental interventions.
Manipulating Organizational Effects
- Neonatal Gonadectomy: Removal of gonads in males or females within the first few days of life to prevent the perinatal hormone surge.
- Hormone Replacement in Neonates: Administering testosterone to neonatal females or an androgen receptor blocker/aromatase inhibitor to neonatal males to test for the organizational role of specific hormone pathways.
Manipulating Activational Effects
- Adult Gonadectomy (GDX): Removal of gonads in adulthood to eliminate circulating sex steroids, followed by assessment of HPA function.
- Steroid Replacement in GDX Adults: Silastic capsule implants or injections are used to provide physiological hormone replacement (e.g., estradiol benzoate, testosterone propionate) to GDX adults, allowing researchers to isolate the activational effects of a specific hormone [105]. Dihydrotestosterone (DHT), a non-aromatizable androgen, can be used to distinguish AR-mediated effects from those requiring conversion to estrogen [105].
Table 3: Key Experimental Interventions and Their Interpretations
| Intervention | Experimental Group | Interpretation of HPA Response vs. Controls |
|---|---|---|
| Neonatal Castration | Male rats castrated at postnatal day 1. | If HPA response is feminized, demonstrates organizational role of perinatal androgens. |
| Testosterone to Neonatal Females | Female rats given testosterone shortly after birth. | If HPA response is masculinized, confirms organizational effect of androgens. |
| Adult Gonadectomy | Adult male or female rats with ovaries/testes removed. | Change in HPA response reveals the nature (inhibitory/facilitatory) of activational hormone effects. |
| Hormone Replacement in GDX Adults | GDX adults given E2, T, or DHT. | Isolates the activational effect of the specific replaced hormone. |
Assessment of HPA Axis Function
- Hormone Measurement: Plasma ACTH and CORT levels are measured via radioimmunoassay (RIA) or ELISA at baseline and at multiple time points after a standardized stressor (e.g., restraint, foot shock, alcohol injection) to characterize the response dynamics [105].
- Gene Expression Analysis: In situ hybridization or RT-PCR is used to quantify CRH and AVP mRNA levels in microdissected PVN tissue [105].
- Neural Activation: Immunohistochemistry for immediate-early genes like c-Fos is used to map stress-activated neurons [104].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Tools for Investigating HPA Sex Differences
| Reagent / Tool | Function / Application | Example from Literature |
|---|---|---|
| Steroid Hormone Implants | Chronic, steady-state hormone replacement in GDX animals. | Innovative Research (Innovative Research of America) steroid pellets (e.g., E121 0.5 mg/pellet; T-111 10 mg/pellet) [105]. |
| Selective AR/ER Modulators | To dissect receptor-specific contributions to activational effects. | Use of non-aromatizable DHT to isolate AR effects [105]. |
| c-Fos Antibodies | Immunohistochemical marker for neuronal activation following stress. | Used to demonstrate greater stress-induced PVN activation in females [104]. |
| CRH and AVP Riboprobes | For in situ hybridization to quantify hypothalamic peptide mRNA. | Demonstrated E2-induced increases in CRH and AVP mRNA in PVN [105]. |
| ACTH & CORT ELISA/RIA Kits | High-throughput measurement of hormone levels in plasma/saliva. | Used to establish greater peak and integrated hormone response in females [104] [105]. |
| CRF-BP Ligand Binding Assays | To study the regulation of CRF bioavailability. | CRF-BP binds CRF with high affinity and modulates HPA axis activity [62]. |
The evidence overwhelmingly confirms that both organizational and activational effects of gonadal hormones are pivotal in establishing and maintaining sex differences in HPA axis responsiveness. The model that emerges is one where perinatal androgens organize a male-typical brain circuit that supports a blunted HPA response, which is subsequently maintained in adulthood by the activational effects of testosterone. The female-typical pattern, organized by the relative absence of perinatal androgens, is potentiated in adulthood by estradiol.
Future research must further elucidate the role of sex chromosomes independent of gonadal hormones, a area that remains relatively unexplored [104]. Furthermore, the interaction between the HPA axis and the hypothalamic-pituitary-gonadal (HPG) axis under conditions of chronic stress is complex and requires deeper investigation, as prolonged HPA activation can suppress gonadal function, thereby altering the hormonal milieu that modulates the stress response [62]. A more complete understanding of these mechanisms will be crucial for developing novel, sex-specific therapeutic strategies for the wide array of stress-related disorders that show a female bias, including depression, anxiety, and autoimmune conditions [104] [7].
The hypothalamic-pituitary-adrenal (HPA) axis and the gut-brain axis represent two critical, interconnected biological systems that play a fundamental role in the pathophysiology of major depressive disorder (MDD). Emerging clinical and preclinical evidence demonstrates that chronic stress induces HPA axis dysregulation, leading to hypercortisolemia, impaired negative feedback, and subsequent neuronal damage in key brain regions including the hippocampus and prefrontal cortex. Simultaneously, stress-induced gut dysbosis disrupts intestinal barrier integrity, promotes systemic inflammation, and alters neurotransmitter production, collectively contributing to depressive symptomatology. This review synthesizes current understanding of the bidirectional communication between these axes, detailing the neuroendocrine, immune, humoral, and neural pathways that facilitate their interaction. Advanced therapeutic strategies targeting the HPA-gut-brain axis, including psychobiotics, fecal microbiota transplantation, and dietary interventions, offer promising avenues for developing novel antidepressant treatments. Elucidating these complex interactions provides a more holistic framework for understanding MDD pathophysiology and developing targeted, personalized interventions.
Major depressive disorder (MDD) remains a debilitating psychiatric condition with profound personal and socioeconomic impacts globally, affecting approximately 280 million individuals annually and representing a leading cause of disability worldwide [107] [15]. Despite widespread use of conventional antidepressants, over one-third of patients exhibit poor or minimal response to these treatments, highlighting the incomplete understanding of depression's underlying pathophysiology and the urgent need for alternative therapeutic targets [107]. Traditionally, depression research has focused on neurotransmitter imbalances, particularly involving serotonin, norepinephrine, and dopamine. However, contemporary understanding has expanded to include broader biological pathways, notably the hypothalamic-pituitary-adrenal (HPA) axis and the gut-brain axis, and their intricate interactions in mediating stress responses and mood regulation [15].
The HPA axis serves as the body's primary neuroendocrine stress response system, regulating cortisol release in response to psychological and physical stressors [28] [7]. Chronic stress can lead to HPA axis overactivation, resulting in elevated cortisol levels that contribute to neuronal damage, particularly in brain regions crucial for mood regulation such as the hippocampus and prefrontal cortex [15]. Concurrently, the gut-brain axis represents a bidirectional communication network between the gastrointestinal tract and the central nervous system that integrates neural, endocrine, immune, and metabolic signaling pathways [108] [109]. The gut microbiota, comprising trillions of microorganisms, influences brain function and behavior through multiple mechanisms, including neurotransmitter production, immune regulation, and maintenance of intestinal barrier integrity [107] [30].
This review explores the integrated HPA-gut-brain axis in depression, examining clinical evidence, mechanistic insights, and therapeutic implications. We synthesize findings from preclinical and clinical studies that establish the microbiota-gut-brain axis (MGBA) as a critical determinant in depression pathogenesis, with particular focus on how gut microbiota alterations impact neuroendocrine, neuroimmune, and metabolic pathways [107]. The complex interplay between these systems offers a more holistic framework for understanding MDD pathophysiology and developing targeted, personalized interventions that extend beyond conventional neurotransmitter-based models.
HPA Axis Dysregulation in Depression
Physiological HPA Axis Function
The HPA axis is a neuroendocrine system composed of hormones, signaling pathways, and feedback loops that regulate various physiological processes, with stress response being one of its primary functions [61]. The axis activation begins in the paraventricular nucleus (PVN) of the hypothalamus with the release of corticotropin-releasing hormone (CRH). CRH then acts on the anterior pituitary gland to stimulate the secretion of adrenocorticotropic hormone (ACTH), which subsequently travels through the bloodstream to the adrenal cortex, specifically targeting the zona fasciculata to induce cortisol production [61]. This system is regulated by a negative feedback mechanism, where both ACTH and cortisol act as inhibitors of CRH and ACTH secretion, thereby maintaining homeostasis [61].
Cortisol secretion follows a pulsatile and oscillatory pattern according to the circadian rhythm, with additional surges occurring in response to stressful stimuli [61]. Neurons in the PVN receive sensory input through several relays, including from the amygdala, a key brain structure involved in processing fear and emotions. This network ensures that emotional or psychological stressors can trigger HPA axis activation and subsequent cortisol release [61]. Under physiological conditions, cortisol exerts anti-inflammatory actions through complex mechanisms that include binding to intracellular glucocorticoid receptors (GRs) and regulating gene transcription [61]. It maintains immune homeostasis by regulating leukocyte trafficking, reducing pro-inflammatory cytokine secretion, and inhibiting the proliferation of T and B lymphocytes [82] [61].
HPA Axis Dysregulation in MDD
In patients with MDD, hyperactivity of the HPA axis is frequently observed, resulting in elevated and persistent cortisol levels [15]. While cortisol is necessary for an adaptive stress response, its chronic and excessive production can have neurotoxic effects, including reduced hippocampal volume, a brain area crucial for emotional regulation and memory [15]. Under normal conditions, high cortisol levels should activate negative feedback mechanisms to inhibit further production of this hormone. However, in individuals with MDD, this negative feedback is often altered, resulting in sustained activation of the HPA axis and perpetuation of the hypercortisolism state [15].
Chronic stress leads to impaired HPA axis feedback, glucocorticoid receptor resistance, and paradoxical cortisol dysregulation, fostering a pro-inflammatory state [7] [61]. Over time, the initial state of hypercortisolism may evolve into adrenal gland adaptive changes, including reduced responsiveness of the adrenal cortex to ACTH and other regulatory stimuli, resulting in a diminished capacity to produce adequate amounts of cortisol - a functional impairment referred to as adrenal resistance or adrenal exhaustion [61]. This HPA axis dysregulation not only impacts how the immune system responds to stressors but also shifts the immune environment toward autoimmunity and inflammation, processes increasingly implicated in depression pathophysiology [7] [61].
Table 1: HPA Axis Alterations in Major Depressive Disorder
| Parameter | Normal Function | MDD Alteration | Consequence |
|---|---|---|---|
| Cortisol Rhythm | Pulsatile, circadian pattern | Disrupted rhythm, elevated baseline | Sleep disturbances, metabolic changes |
| Negative Feedback | Intact GR-mediated feedback | Impaired feedback sensitivity | Sustained cortisol secretion |
| Receptor Sensitivity | Normal GR expression and function | Glucocorticoid resistance | Reduced anti-inflammatory effects |
| Hippocampal Volume | Maintained structural integrity | Volume reduction | Impaired memory, emotional regulation |
| Immune Regulation | Balanced inflammatory control | Pro-inflammatory state | Increased cytokine production |
Gut-Brain Axis in Depression
Gut Microbiota and Brain Communication
The gut-brain axis represents a bidirectional communication network between the gastrointestinal tract and the central nervous system that involves complex neurochemical, immunological, and hormonal interactions [108] [15]. The human gut microbiota, comprised of trillions of microorganisms, acts as a "second brain," influencing central nervous system function through multiple pathways previously underrecognized [107]. Gut microbes not only participate in food digestion but also synthesize neurotransmitters such as serotonin, dopamine, and GABA (gamma-aminobutyric acid), which are crucial for regulating mood and anxiety [15]. Notably, approximately 90% of the body's serotonin is produced in the gut, highlighting the importance of this pathway for mental health [15].
The communication between the gut and brain occurs through four major pathways: (1) the neurologic pathway, including the vagus nerve, enteric nervous system, and neurotransmitter activity; (2) the endocrine pathway, involving gut microbiota alteration of nutrient availability and biologically active peptides from enteroendocrine cells; (3) the humoral/metabolic pathway, featuring bacterial metabolites such as short-chain fatty acids (SCFAs) and lipopolysaccharide (LPS); and (4) the immune pathway, involving cytokine release and other immune mediators [108]. These communication pathways allow the brain to influence intestinal activities, including functional immune effector cells, and the gut to influence mood, cognition, and mental health [108].
Gut Dysbiosis in Depression
Intestinal dysbiosis, an imbalance in the composition of gut bacteria, has been consistently associated with the development of mood disorders, including MDD [107] [15]. Both clinical and preclinical studies show significant microbial composition changes during depressive states [107]. Individuals with depression often exhibit an altered gut microbiome compared to healthy controls, characterized by changes in the abundance of specific bacterial taxa [107] [28]. For instance, some studies have reported increased abundance of Firmicutes, whereas the abundance of Bacteroidetes was decreased in subsets of patients with depression and related conditions [28].
This imbalance can increase intestinal permeability, allowing bacterial components such as lipopolysaccharides (LPS) to enter the systemic circulation, which triggers a chronic inflammatory response that can have deleterious effects on the CNS [108] [15]. Pro-inflammatory cytokines such as interleukin (IL)-6 and tumor necrosis factor-alpha (TNF-α) can cross the blood-brain barrier, negatively influencing neuroplasticity and neuronal function, thereby contributing to depressive symptomatology [15]. The causal role of microbiota in depression development has been demonstrated by fecal transplantation studies, where transplantation of microbiota from depressed patients to rodents induces depression-like behavior [107] [28].
Integrated HPA-Gut-Brain Axis Mechanisms
Bidirectional Interactions
The HPA and gut-brain axes do not function in isolation but are intricately interconnected, with their interaction being central to understanding MDD pathophysiology [15]. Chronic stress activates the HPA axis, leading to increased cortisol release, which can directly alter gut microbiota composition and increase intestinal permeability [28] [108]. This impaired barrier function allows bacterial translocation and systemic immune activation, further exacerbating HPA axis dysregulation through pro-inflammatory cytokine signaling [28] [30]. This creates a vicious cycle wherein stress-induced HPA activation promotes gut dysbiosis and intestinal barrier dysfunction, which in turn amplifies systemic inflammation and neuroinflammation, further driving depressive pathology [15] [30].
The gut microbiota significantly influences HPA axis development and function. Germ-free mice exhibit enhanced HPA response to stress, with significantly increased ACTH and corticosterone levels after restraint stress compared to specific pathogen-free mice [108]. This hyperresponsive HPA axis in germ-free animals can be normalized by reconstitution with specific bacteria, such as Bifidobacterium infantis, demonstrating the critical role of microbiota in HPA axis programming [108]. Additionally, gut microbes regulate the set point for HPA axis activity through effects on central corticosteroid receptors, with microbiota influencing glucocorticoid receptor expression in key brain regions involved in HPA feedback inhibition, including the hippocampus and hypothalamus [28].
Key Molecular Mechanisms
Several key molecular mechanisms mediate the interaction between the HPA and gut-brain axes in depression:
Neuroendocrine Signaling: Gut microbiota alterations affect the HPA axis through multiple neuroendocrine pathways. Microbial metabolites, including short-chain fatty acids (SCFAs) such as butyrate and propionate, can modulate HPA activity directly or indirectly through effects on enteroendocrine cells and gut hormone release [28] [108]. SCFAs also influence cortisol secretion from the adrenal cortex and norepinephrine release from the adrenal medulla, demonstrating direct involvement in the HPA axis response to stress [108].
Immune Activation: Gut dysbiosis promotes increased intestinal permeability, allowing bacterial lipopolysaccharide (LPS) to enter the systemic circulation and trigger immune activation [108] [30]. This results in elevated pro-inflammatory cytokines (e.g., IL-1β, IL-6, TNF-α), which can cross the blood-brain barrier and activate microglia, leading to neuroinflammation [107] [15]. These inflammatory mediators are potent activators of the HPA axis, creating a feed-forward loop that perpetuates both HPA dysregulation and inflammatory signaling [28] [61].
Neurotransmitter Systems: Gut microbiota significantly influence serotonin synthesis, with approximately 90% of the body's serotonin produced in the gut [15]. Microbial regulation of tryptophan metabolism, the primary serotonin precursor, represents a crucial pathway through which gut microbes can affect central serotonin signaling and depressive behaviors [99]. Additionally, gut microbes produce various neuroactive compounds, including GABA, dopamine, and acetylcholine, which can directly or indirectly influence brain function and behavior [108] [109].
Neurotrophic Factors: The microbiota-gut-brain axis regulates the expression of brain-derived neurotrophic factor (BDNF), a key protein involved in neuronal plasticity and cognition [108]. Germ-free mice show reduced BDNF expression in the cortex and hippocampus, which can be reversed by microbial colonization [108]. Chronic stress reduces BDNF levels, contributing to hippocampal atrophy, while antidepressant treatments and certain probiotics can increase BDNF expression, promoting neuroplasticity and resilience [108] [15].
Table 2: Key Experimental Models for Studying HPA-Gut-Brain Axis in Depression
| Model Type | Key Features | Measured Parameters | Relevance to Human MDD |
|---|---|---|---|
| Chronic Unpredictable Mild Stress (CUMS) | Series of unpredictable, mild stressors | Depression-like behaviors, HPA activity, microbiota changes | Mimics chronic low-grade stress in humans |
| Chronic Social Defeat Stress (CSDS) | Repeated social subjugation by dominant conspecific | Social withdrawal, anhedonia, gut dysbiosis | Models psychological and social stressors |
| Maternal Separation (MS) | Early life stress through pup separation | Gut microbiome disruption, neuroimmune activation | Represents early life adversity risk factor |
| Germ-Free (GF) Animals | Raised in sterile conditions without microbiota | HPA stress response, neurotransmitter levels, BDNF | Isulates microbiota contribution to development |
| Fecal Microbiota Transplantation (FMT) | Transfer of microbiota from donors to recipients | Behavior transfer, physiological changes | Establishes causality in gut-brain communication |
Experimental Evidence and Methodologies
Preclinical Studies
Preclinical models have been instrumental in elucidating the causal relationships between gut microbiota, HPA axis function, and depressive-like behaviors. A widely employed animal model in this research is the chronic unpredictable mild stress (CUMS) model, which induces stress-related behaviors by exposing animals to a series of unpredictable, mild stressors, mimicking the symptoms of depression [107]. In mice subjected to CUMS, significant alterations in the gut microbiota occur, including an increase in Proteobacteria and Verrucomicrobia, coupled with a decrease in beneficial bacteria such as Bifidobacteriaceae and Lactobacillaceae [107]. Notably, fecal microbiota transplantation (FMT) from CUMS mice to healthy recipients successfully replicates depressive phenotypes, establishing a direct link between gut dysbiosis and depression [107].
The chronic social defeat stress (CSDS) model is another frequently used animal model to study depression, specifically targeting psychological and social stressors that contribute to depressive behaviors [107]. Mice exposed to CSDS display significant gut microbiota dysbiosis, characterized by reduced alpha diversity and a notable decline in Lactobacillus abundance [107]. These microbial changes are linked to metabolic and immune-modulatory functions that may influence the stress response and contribute to depressive behaviors [107].
Germ-free (GF) animal models have provided fundamental insights into the essential role of microbiota in brain development and function. GF mice exhibit an exaggerated HPA axis response to stress, with significantly increased ACTH and corticosterone levels after acute stress compared to conventionally colonized mice [28] [108]. This HPA hyper-reactivity in GF mice is associated with reduced BDNF expression in the cortex and hippocampus, and can be reversed by microbial colonization, particularly if performed during early life [108]. These findings highlight the critical role of microbiota in the developmental programming of the HPA axis and stress responsiveness.
Clinical Evidence
Clinical studies have reinforced preclinical findings, showing that individuals with depression often have an altered gut microbiome compared to healthy controls [107] [28]. While no definitive microbial signature for depression has yet been established, consistent alterations have been observed, including changes in the abundance of Firmicutes and Bacteroidetes [28]. A causal role of the microbiota in depression development has been demonstrated by fecal transplantation studies in humans. Transplantation of microbiota from depressed patients to rodents induces depression-like behavior and anhedonia, accompanied by indices of immune activation [28] [99].
Several small trials of probiotics for depression have found positive effects. A meta-analysis of seven such trials found that probiotics—known as psychobiotics when used to improve mental health—are effective as an add-on to standard treatments, but not when used alone [99]. A pilot trial of 49 people with depression who had previously had only a partial response to antidepressants found that those receiving a multistrain probiotic in addition to their medication for eight weeks showed greater reductions in depression and anxiety-related symptoms compared with the placebo group [99].
Fecal microbiota transplantation (FMT) has shown promising results in early trials. In one trial for treatment-resistant depression, participants like Andrew Moseson reported transformative improvements, with benefits emerging within about a week and sustained over two years [99]. The trial leader, psychiatrist Valerie Taylor, noted that if comprehensive microbiota alterations via FMT can demonstrate efficacy, it provides justification for pursuing more targeted probiotic interventions [99].
Therapeutic Implications and Future Directions
Microbiota-Targeted Interventions
The understanding of HPA-gut-brain axis interactions in depression has opened promising avenues for novel therapeutic interventions:
Psychobiotics: These are probiotics with potential mental health benefits when administered in adequate amounts. The most promising psychobiotics for depression include strains of Lactobacillus and Bifidobacterium, which have shown efficacy in alleviating depressive symptoms in both animal models and human trials [99]. Psychobiotics typically exert their effects through multiple mechanisms, including regulation of the HPA axis, reduction of pro-inflammatory cytokines, increased production of neurotrophic factors, and enhancement of neurotransmitter signaling [107] [99]. Current evidence suggests psychobiotics are most effective as adjunctive therapies alongside conventional antidepressants rather than as stand-alone treatments [99].
Fecal Microbiota Transplantation (FMT): FMT involves transferring stool from a healthy donor to a recipient to restore a healthy balance of gut bacteria [107] [99]. Early trials in depression have shown transformative results for some individuals with treatment-resistant depression, with benefits emerging rapidly and sustained over extended periods [99]. While FMT demonstrates the therapeutic potential of comprehensive microbiota alterations, it does little to narrow down which specific microbes are responsible for the benefits, limiting its clinical scalability and safety profile [99].
Dietary Interventions: Dietary modifications represent a broad-spectrum approach to modulating the gut microbiota and supporting mental health. A study published in 2017 found that an intervention based on a Mediterranean diet reduced symptoms in people with depression [99]. Dietary changes affect the broader microbial ecosystem by introducing many compounds that microbes feed on (prebiotics), supporting the growth of beneficial taxa that produce anti-inflammatory metabolites and neurotransmitters [99].
HPA Axis-Targeted Approaches
Conventional antidepressants themselves can modulate HPA axis function, with effective treatments often restoring normal HPA feedback regulation and reducing cortisol levels over time [15]. Additionally, specific HPA-targeted therapies are under investigation:
CRH Receptor Antagonists: These compounds block the action of corticotropin-releasing hormone, the initial driver of HPA axis activation, potentially normalizing the stress response system in depression [15].
Glucocorticoid Receptor Modulators: These agents aim to restore normal glucocorticoid receptor function and improve negative feedback inhibition of the HPA axis [61].
Non-pharmacological Approaches: Stress reduction techniques such as mindfulness-based therapies, cognitive-behavioral therapy, and regular exercise can normalize HPA axis function and positively influence gut microbiota composition, representing integrative approaches to modulating the HPA-gut-brain axis [15] [82].
Research Gaps and Future Perspectives
Despite significant advances, several challenges remain in translating HPA-gut-brain axis research into clinical practice. These include the lack of standardization in probiotic formulations, limited understanding of optimal strains and dosages for specific depressive subtypes, and insufficient mechanistic knowledge about how microbiota-based interventions exert their effects [107] [99]. Additionally, the field lacks validated biomarkers to identify patients most likely to benefit from microbiota-targeted therapies and to monitor treatment response [99].
Future research should focus on large-scale human trials with integrated mechanism investigations to identify which pathways are activated in which disorders, in what relative contribution, and at what point in life [99]. Multi-omics approaches combining metagenomics, metabolomics, and proteomics will be essential for understanding the functional consequences of microbial changes rather than just compositional shifts [107] [30]. Personalized medicine approaches that account for individual microbiome and immune profiles will likely be necessary, given the high variability in microbial composition between individuals and the functional redundancy within microbial communities [99] [30].
Table 3: Research Reagent Solutions for HPA-Gut-Brain Axis Investigations
| Research Tool Category | Specific Examples | Key Applications | Technical Considerations |
|---|---|---|---|
| Animal Models | CUMS, CSDS, Maternal Separation, Germ-Free | Stress pathophysiology, causality testing | Standardization of protocols, translational validity |
| Microbiome Analysis | 16S rRNA sequencing, metagenomics, metabolomics | Microbial composition and functional potential | Sample collection standardization, bioinformatics |
| HPA Axis Assessment | CORT/ACTH ELISA, dexamethasone suppression test | HPA activity and feedback integrity | Circadian timing, stress-free collection methods |
| Gut Barrier Function | FITC-dextran assay, zonulin measurements, tight junction markers | Intestinal permeability assessment | Tissue processing standardization, confounding factors |
| Neuroinflammation Assays | Cytokine profiling, microglial activation markers, GFAP IHC | CNS immune activation evaluation | Region-specific analyses, post-mortem intervals |
The HPA-gut-brain axis represents a fundamental biological framework for understanding the complex pathophysiology of major depressive disorder. The bidirectional communication between these systems creates a series of feedback loops wherein chronic stress drives HPA axis dysregulation and cortisol imbalance, which in turn promotes gut dysbiosis, intestinal barrier dysfunction, and systemic inflammation that further exacerbates neuroendocrine and neuroimmune disturbances. This integrated perspective moves beyond traditional neurotransmitter-centric models of depression to encompass neuroendocrine, immune, metabolic, and microbial dimensions of the disorder.
The therapeutic implications of this expanded understanding are substantial, offering novel approaches for managing depression through microbiota-targeted interventions, HPA axis modulation, and integrative strategies that address both systems simultaneously. While challenges in standardization, mechanistic understanding, and efficacy remain, HPA-gut-brain axis-centered approaches represent a promising shift toward microbiota-based diagnostics and personalized treatments for depression. Future research focusing on large-scale human trials with integrated mechanism investigations will be essential for translating these promising findings into effective clinical applications that address the multifaceted nature of depression.
The hypothalamic-pituitary-adrenal (HPA) axis represents the body's primary neuroendocrine stress response system, integrating neural, endocrine, and immune signals to maintain homeostasis under challenging conditions. In both rodents and humans, psychological stress activates the paraventricular nucleus (PVN) of the hypothalamus to release corticotropin-releasing hormone (CRH), which stimulates anterior pituitary secretion of adrenocorticotropic hormone (ACTH). This ultimately drives adrenal production of glucocorticoids (corticosterone in rodents, cortisol in humans) that regulate diverse physiological processes including immune function, metabolism, and cognition [81] [17].
Under conditions of chronic stress, this carefully orchestrated system becomes dysregulated, leading to impaired negative feedback, glucocorticoid receptor resistance, and paradoxical cortisol dysregulation that fosters a pro-inflammatory state [81]. This HPA axis dysregulation constitutes a critical mechanistic link between psychological stress and various disease states, particularly autoimmune conditions and mood disorders [81] [17]. The translational challenge lies in identifying biomarkers that accurately reflect these complex neuroendocrine-immune interactions across species barriers, enabling effective translation of rodent model findings to human pathophysiology and therapeutic development.
HPA Axis Physiology and Stress-Induced Dysregulation
Normative HPA Axis Functioning
The HPA axis operates through a sophisticated cascade of hormonal signaling events characterized by pulsatile, circadian rhythms. Under basal conditions, cortisol secretion follows a natural oscillatory pattern that synchronizes immune responses and maintains homeostasis [81]. The system is regulated by a precise negative feedback mechanism wherein both ACTH and cortisol inhibit further CRH and ACTH secretion, maintaining physiological balance [81]. Cortisol exerts its effects primarily through binding to intracellular glucocorticoid receptors (GRs), modulating gene expression by suppressing pro-inflammatory signaling pathways involving transcription factors such as NF-κB and AP-1 [81]. This results in decreased production of pro-inflammatory cytokines (including IL-1β, IL-6, and TNF-α), chemokines, and other immune-activating molecules [81].
Pathological Dysregulation Under Chronic Stress
Chronic stress triggers maladaptive changes in HPA axis function through multiple mechanisms. Persistent activation leads to loss of normal pulsatile and circadian rhythms, impaired negative feedback mechanisms, and altered receptor sensitivity [81]. Over time, the initial state of hypercortisolism may evolve into adrenal exhaustion, characterized by reduced responsiveness of the adrenal cortex to ACTH and diminished cortisol production capacity [81]. This dysregulation creates a pro-inflammatory state through several pathways: diminished immunosuppressive effects, increased mineralocorticoid receptor activation promoting pro-inflammatory gene expression, and weakened protective immune mechanisms that collectively shift the immune environment toward autoimmunity and inflammation [81] [17].
Table 1: Key Hormonal Components of the HPA Axis and Their Functions
| Component | Origin | Primary Function | Regulatory Role |
|---|---|---|---|
| Corticotropin-Releasing Hormone (CRH) | Paraventricular Nucleus of Hypothalamus | Initiates HPA axis cascade | Stimulates ACTH release from anterior pituitary |
| Adrenocorticotropic Hormone (ACTH) | Anterior Pituitary | Adrenal cortex stimulation | Drives cortisol/corticosterone production |
| Cortisol (Humans)/Corticosterone (Rodents) | Adrenal Cortex | Primary glucocorticoid effectors | Anti-inflammatory effects, metabolic regulation, negative feedback |
| Glucocorticoid Receptors (GR) | Intracellular; widespread distribution | Mediate genomic effects of cortisol | Regulate gene transcription; suppress pro-inflammatory pathways |
Translational Biomarker Platforms: From Rodent Models to Human Applications
Neuroimaging Intermediate Phenotypes
Resting-state functional magnetic resonance imaging (fMRI) has emerged as a powerful translational tool for identifying neural intermediate phenotypes that bridge rodent models and human depression. Research has demonstrated distinct amplitude of low-frequency fluctuations (ALFF) patterns in genetic (P11 knockout mice) versus environmental stress (chronic unpredictable mild stress) rodent models [110]. These patterns are conserved in human depression subtypes, enabling classification based on etiological mechanisms rather than solely behavioral manifestations [110].
The genetic subtype (P11 KO-like) shows higher polygenic risk scores for major depressive disorder with enriched risk gene expression in brain tissues and abnormal metabolites linked to tryptophan metabolism. In contrast, the stress animal-like subtype does not show changes in genetic risk scores but exhibits enriched risk gene expression in somatic and endocrine tissues with mitochondrial dysfunction in the antioxidant stress system [110]. These distinct neuroimaging patterns successfully predict anhedonia, a core symptom of depression, in both rodent models and human subtypes, validating their utility as translational biomarkers [110].
Figure 1: Cross-Species Validation of Neuroimaging Biomarkers for Depression Subtyping
Molecular and Genetic Biomarkers
Advances in genomic technologies have enabled identification of molecular biomarkers that track stress vulnerability and resilience across species. The FKBP5 gene, a regulator of glucocorticoid receptor sensitivity, has been consistently validated as a stress biomarker, with polymorphisms influencing HPA axis function and depression risk [111]. Other promising biomarkers with strong convergent functional evidence include DDX6, B2M, LAIR1, RTN4, and NUB1 [111].
Transcriptomic profiling from peripheral blood samples has identified gene expression signatures predictive of high-stress states and future psychiatric hospitalizations. Notably, these biomarkers demonstrate improved predictive accuracy when personalized by gender and psychiatric diagnosis [111]. Emerging evidence also implicates epigenetic modifications, particularly DNA methylation of the serotonin transporter gene (SLC6A4), as a biomarker of stress exposure and HPA axis reactivity [112].
Table 2: Validated and Emerging Biomarkers in Stress Pathophysiology
| Biomarker Category | Specific Markers | Functional Significance | Translational Evidence |
|---|---|---|---|
| Genetic | FKBP5 polymorphisms | Glucocorticoid receptor sensitivity, HPA axis feedback | Strong human genetic association; rodent mechanistic studies |
| Transcriptomic | NUB1, APOL3, MAD1L1, NKTR | Cellular stress response pathways | Predictive of high-stress states and hospitalization risk |
| Epigenetic | SLC6A4 methylation | Serotonin signaling regulation | Associated with elevated cortisol stress response |
| Neuroimaging | ALFF patterns in subcortical-sensorimotor regions | Neural circuit dysfunction | Cross-species validation in genetic vs. stress models |
| Inflammatory | IL-6, TNF-α, CRP | Pro-inflammatory cytokine activity | Elevated in chronic stress and depression across species |
| Metabolomic | Tryptophan metabolism intermediates | Serotonin synthesis, mitochondrial function | Distinct patterns in genetic vs. stress-related depression |
Experimental Protocols and Methodologies
Rodent Models of Stress Pathophysiology
Chronic Unpredictable Mild Stress (CUMS) Protocol
- Animals: Male Sprague-Dawley rats (approximately 3 months old), housed under standard conditions with ad libitum access to food and water except where specified as a stressor.
- Stress Regimen: Animals are exposed to various mild stressors in an unpredictable sequence over 4-8 weeks. Stressors include: 12-hour food deprivation, 12-hour water deprivation, continuous overnight illumination, cage tilt (45°), soiled cage (200 mL water in bedding), paired housing, exposure to empty water bottles, and brief restraint stress.
- Behavioral Assessments:
- Sucrose Preference Test (SPT): Measures anhedonia by calculating preference for 1% sucrose solution over water during a 4-hour period after 12-hour water deprivation.
- Forced Swim Test (FST): Assesses behavioral despair by measuring immobility time during a 5-minute test in inescapable water-filled cylinder.
- Open Field Test (OFT): Evaluates anxiety-like behavior and locomotor activity by tracking movement in a novel arena.
- Neuroimaging: Whole-brain fMRI data acquired using gradient-echo echo-planar imaging (GE EPI) sequence to measure ALFF under isoflurane anesthesia [110].
Genetic Model (P11 Knockout Mice)
- Animals: P11 KO mice and wild-type C57BL/6J controls, male, 10-12 weeks old at testing.
- Genotyping: Confirm P11 knockout status via PCR of tail DNA.
- Behavioral Battery: Identical tests to CUMS model (SPT, FST, OFT) to enable cross-model comparison.
- Molecular Analyses: Post-mortem tissue collection for Western blot, qPCR, and immunohistochemistry to validate target engagement and downstream molecular effects [110].
Human Translational Studies
Cohort Design and Clinical Assessments
- Participant Recruitment: Multi-site recruitment of patients with major depressive disorder and healthy controls across appropriate age ranges (typically 18-65).
- Clinical Characterization:
- Structured Clinical Interviews: DSM-5 criteria for depression and comorbid conditions.
- Symptom Severity: 17-item Hamilton Depression Rating Scale (HAMD-17) for overall severity.
- Anhedonia Specificity: Snaith-Hamilton Pleasure Scale (SHAPS) for reward processing deficits.
- Stress Measures: Simplified Stress Scale (visual analog scale for life, financial, health, social stress) and PTSD Checklist-Civilian Version (PCL-C) for trauma-related symptoms [111] [110].
- Biospecimen Collection: Whole blood (10 mL) in PAXgene tubes for RNA extraction and gene expression studies; plasma/serum for cortisol and inflammatory markers.
Neuroimaging Acquisition and Analysis
- Image Acquisition: 3T MRI scanners with standardized parameters across sites: T1-weighted structural images and resting-state fMRI (eyes open, fixating) with 8-channel head coils.
- Preprocessing Pipeline: Standardized processing using DPABI or similar toolbox, including realignment, normalization, smoothing, and ALFF calculation.
- Subtyping Approach: t-distributed Stochastic Neighbor Embedding (t-SNE) for dimensionality reduction followed by agglomerative hierarchical clustering to identify neuroimaging subtypes [110].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Stress Biomarker Investigations
| Reagent/Category | Specific Examples | Research Application | Translational Utility |
|---|---|---|---|
| Genetic Analysis | FKBP5 genotyping assays, RT-PCR primers for stress-related genes | Genetic association studies, gene expression quantification | Cross-species conservation of stress pathways enables direct translation |
| Protein Assays | Cortisol/ACTH ELISAs, multiplex cytokine panels (IL-6, TNF-α, CRP) | HPA axis hormone measurement, inflammatory profiling | Identical assays adaptable for rodent and human samples |
| Neuroimaging | ALFF analysis pipelines, 3D ResNet classification algorithms | Neural circuit identification, automated subtype classification | Consistent metrics across species (rodent 7T/9.4T to human 3T) |
| Epigenetic Tools | SLC6A4 methylation arrays, chromatin immunoprecipitation kits | DNA methylation analysis, transcription factor binding studies | Mechanism linking environmental stress to stable molecular changes |
| Behavioral Assays | Sucrose preference test apparatus, forced swim test equipment | Anhedonia assessment, behavioral despair measurement | Conserved behavioral readouts across rodent and human studies |
Integrated Signaling Pathways in Stress Pathophysiology
Figure 2: Integrated Neuroendocrine-Immune Signaling in Chronic Stress
The pathophysiology of stress involves complex bidirectional communication between the central nervous system and peripheral systems. Psychological stressors activate amygdala inputs to hypothalamic PVN neurons, initiating the HPA axis cascade through CRH and ACTH signaling that ultimately drives cortisol production [81] [17]. Under acute conditions, cortisol exerts anti-inflammatory effects and maintains homeostasis. However, chronic exposure leads to glucocorticoid receptor resistance, impairing negative feedback and creating a pro-inflammatory state characterized by elevated IL-6, TNF-α, and other inflammatory mediators [81] [17].
Simultaneously, stress-induced gut-brain axis dysregulation promotes increased intestinal permeability, allowing bacterial endotoxins (e.g., LPS) to enter circulation and further stimulate immune activation [15]. This systemic inflammation can cross the blood-brain barrier, contributing to neuroinflammation, reduced hippocampal neurogenesis, and prefrontal cortex dysfunction—key neural substrates underlying stress-related psychiatric disorders [15] [17]. The resulting neuronal damage and glucocorticoid resistance complete a vicious cycle that perpetuates HPA axis dysregulation and maintains the pathological state.
Translational biomarkers represent the critical bridge between rodent models of stress pathophysiology and human neuropsychiatric disorders. The integration of multi-omics approaches (genomic, transcriptomic, epigenomic, metabolomic) with neuroimaging intermediate phenotypes and behavioral assessments provides a comprehensive framework for deconstructing the heterogeneity of stress-related disorders [112] [110]. The consistent identification of distinct biological subtypes—particularly the differentiation between genetically-driven and stress-induced depression phenotypes—offers promising avenues for personalized therapeutic approaches.
Future research should prioritize longitudinal study designs that track biomarker dynamics across stress vulnerability, resilience, and disease progression timelines. Additionally, greater emphasis on circuit-level analyses mapping specific neuronal populations that regulate brain-body communication will enhance our understanding of how psychological stressors translate into peripheral pathophysiology [17]. The development of advanced computational methods for integrating diverse biomarker modalities will be essential for creating predictive models of individual stress trajectories and treatment responses. As these biomarker platforms mature, they hold tremendous potential for transforming the precision diagnosis and treatment of stress-related disorders, ultimately enabling targeted interventions that address the unique biological signature of each patient's condition.
The hypothalamic-pituitary-adrenal (HPA) axis represents a critical neuroendocrine interface between the brain and the body's stress response system, making it a promising therapeutic target for a spectrum of stress-related disorders. Dysregulation of this axis has been implicated in the pathophysiology of major depressive disorder (MDD), post-traumatic stress disorder (PTSD), anxiety disorders, and autoimmune conditions, characterized by altered cortisol dynamics and impaired feedback mechanisms [7] [113]. The development of HPA-targeted interventions requires specialized clinical trial methodologies that account for the axis's complex physiology, circadian rhythmicity, and interaction with other biological systems. This technical guide provides a comprehensive framework for validating the efficacy of HPA-targeted interventions, encompassing pharmacological and non-pharmacological approaches, with specific consideration of experimental designs, endpoint measurements, and analytical approaches tailored to this unique therapeutic domain.
HPA Axis Physiology and Pathophysiology
Core Components and Signaling Pathways
The HPA axis functions as a neuroendocrine circuit that regulates the body's adaptation to physical and psychological stressors. The cascade begins with corticotropin-releasing factor (CRF) and arginine vasopressin (AVP) secretion from parvocellular neurons of the hypothalamic paraventricular nucleus (PVN) [62] [3]. These peptides stimulate anterior pituitary corticotropes to release adrenocorticotropic hormone (ACTH) into systemic circulation. ACTH subsequently acts on the adrenal cortex to stimulate the synthesis and secretion of glucocorticoids (cortisol in humans, corticosterone in rodents), which mediate widespread physiological effects through mineralocorticoid receptors (MR) and glucocorticoid receptors (GR) [113] [3]. The axis is regulated by negative feedback mechanisms wherein circulating glucocorticoids inhibit their own secretion through actions at hippocampal, hypothalamic, and pituitary sites.
Mechanisms of HPA Axis Dysregulation
Dysregulation of the HPA axis manifests differently across psychiatric and medical conditions. In major depressive disorder, evidence suggests CRF hypersecretion, impaired negative feedback, and elevated cortisol levels, potentially resulting from reduced GR sensitivity and function [114] [113]. In contrast, PTSD often presents with hypocortisolism and enhanced negative feedback sensitivity, possibly reflecting an adaptive down-regulation following initial trauma exposure [115]. Chronic stress can lead to progressive HPA axis alterations characterized by initial hyperactivity followed by eventual adrenal exhaustion and blunted responsivity [7] [116]. These distinct pathophysiological profiles necessitate disorder-specific therapeutic approaches and validation strategies.
Clinical Trial Endpoints and Biomarkers
Primary Efficacy Endpoints
Validating HPA-targeted interventions requires a multi-dimensional assessment strategy encompassing endocrine, clinical, and functional endpoints. The table below summarizes key biomarkers and their methodological considerations for clinical trials.
Table 1: HPA Axis Biomarkers for Clinical Trials
| Biomarker Category | Specific Measures | Methodological Considerations | Clinical Associations |
|---|---|---|---|
| Basal Hormone Levels | Plasma/salivary cortisol (diurnal profile), ACTH, DHEA(S) | Circadian timing, CAR measurement, sampling duration | Hypercortisolism in MDD, hypocortisolism in PTSD [115] [113] |
| Dynamic Challenge Tests | Dexamethasone suppression test (DST), DEX/CRF test, prednisolone suppression test | Dose timing, pharmacokinetic variables, population norms | Non-suppression indicates impaired feedback in MDD [117] [113] |
| Receptor Function | GR and MR sensitivity via pharmacological challenges | Receptor-specific agonists/antagonists, response kinetics | Reduced GR sensitivity in depression [117] |
| Clinical Endpoints | Disease-specific symptom scales (HAMD, CAPS), remission rates, functional outcomes | Observer-rated vs. self-report, cultural validation | Symptom improvement with HPA normalization [114] [115] |
Neuroendocrine Assessment Protocols
Comprehensive HPA axis assessment requires standardized protocols for sample collection and processing. The cortisol awakening response (CAR) should be measured by collecting saliva or plasma samples immediately upon awakening and at 30, 45, and 60 minutes post-awakening in the participant's natural environment [115]. Diurnal cortisol profiles typically require samples at waking, noon, late afternoon, and bedtime to capture the circadian slope. Pharmacological challenge tests necessitate careful timing relative to drug administration; for example, the dexamethasone suppression test involves administering dexamethasone at 11 PM and measuring cortisol the following day between 8 AM and 4 PM [113]. All samples should be processed promptly with proper preservation to prevent degradation, and documentation of potential confounders (medication, sleep quality, smoking, exercise) is essential for accurate interpretation.
Clinical Trial Designs for HPA-Targeted Interventions
Pharmacological Trial Designs
Proof-of-Concept Trials for HPA-targeted medications should employ randomized, double-blind, placebo-controlled designs with biomarker-stratified populations. Target engagement should be demonstrated through specific HPA axis biomarkers before assessing clinical efficacy. For instance, trials of GR antagonists (e.g., mifepristone) should confirm dose-dependent effects on cortisol signaling prior to evaluating antidepressant effects [114]. Dose-finding studies should incorporate multiple HPA endpoints to establish optimal biological dosing rather than relying solely on tolerability. Phase III trials benefit from enrichment designs that select patients with confirmed HPA axis dysregulation, such as non-suppressors on the DEX/CRF test [113].
Multi-stage trial designs are particularly efficient for HPA-targeted interventions. An initial biomarker stage can confirm target engagement, followed by randomization of only those participants showing adequate biological response to subsequent efficacy stages. This approach increases power while reducing sample size requirements and is especially valuable for targeted therapies where only a subset of patients may exhibit the relevant neuroendocrine abnormality.
Non-Pharmacological Intervention Designs
Psychotherapeutic trials investigating HPA axis modulation present unique methodological challenges. Trauma-focused psychotherapy for PTSD has demonstrated potential to normalize HPA axis function, with studies showing altered cortisol levels and enhanced feedback regulation following successful treatment [115]. These trials should incorporate carefully matched control conditions (e.g., supportive therapy without trauma focus) to isolate specific effects on stress response systems. Timing of endocrine assessments relative to therapy sessions is critical, as acute effects may differ from long-term adaptations.
Mind-body interventions and lifestyle approaches require special consideration of control conditions to account for non-specific effects. Trials should measure HPA parameters at multiple timepoints to capture potential biphasic responses—initial activation followed by adaptation. The table below outlines key considerations for non-pharmacological intervention trials targeting HPA axis function.
Table 2: Trial Designs for Non-Pharmacological HPA-Targeted Interventions
| Intervention Type | Control Condition | Primary HPA Endpoints | Timing Considerations |
|---|---|---|---|
| Psychotherapy (TF-CBT, EMDR) | Supportive therapy, waitlist, cognitive restructuring without exposure | Diurnal cortisol slope, CAR, DST suppression | Pre/post-treatment, follow-up (3-6 months) to assess persistence [115] |
| Mind-Body Interventions (yoga, meditation) | Stress education, light exercise, relaxation training | Awakening cortisol, cortisol stress reactivity, inflammatory markers | Mid-intervention and post-intervention to track progression |
| Gut-Brain Axis (probiotics, prebiotics) | Placebo supplements, isocaloric control | Circulating cortisol, CRP, inflammatory cytokines | Minimum 8-week duration for microbial stabilization [15] |
| Lifestyle Modification (sleep, exercise) | Health education, maintenance of current habits | Diurnal rhythm, GR sensitivity, heart rate variability | Seasonal variations, adherence monitoring |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for HPA Axis Studies
| Reagent Category | Specific Examples | Research Applications | Technical Notes |
|---|---|---|---|
| GR Antagonists | Mifepristone (RU-486) | Proof-of-concept for GR involvement, treatment-resistant depression | 300-1200mg/day doses; monitor liver enzymes [114] |
| Vasopressin Receptor Antagonists | V1B receptor antagonists | Investigating AVP-mediated HPA activation, depressive disorders | Limited clinical availability; research use [114] |
| Steroidogenesis Inhibitors | Metyrapone, ketoconazole | Reducing cortisol production, testing cortisol dependence of pathology | Risk of adrenal insufficiency; rescue protocols needed |
| MR Agonists/Antagonists | Fludrocortisone, spironolactone | Assessing MR contribution to HPA regulation, cognitive function | Blood pressure monitoring essential [117] |
| CRF Receptor Antagonists | Various research compounds | Blocking CRF-mediated signaling, anxiety and depression models | Limited blood-brain barrier penetration for some compounds |
| Synthetic Glucocorticoids | Dexamethasone, prednisolone | Feedback sensitivity tests (DST), receptor selectivity assessment | Prednisolone has mixed MR/GR affinity vs. dexamethasone GR selectivity [117] |
Experimental Protocols and Methodologies
Pharmacological Challenge Protocols
Combined Dexamethasone/CRF Test Protocol: This sophisticated paradigm assesses HPA axis feedback sensitivity and central drive. Participants receive 0.5-1.5mg dexamethasone orally at 11 PM, followed by 1μg/kg human CRF administered intravenously the next day between 2-4 PM [113]. Blood samples for ACTH and cortisol measurement are collected at -30, 0, +15, +30, +45, +60, +90, and +120 minutes relative to CRF administration. The test is particularly sensitive to HPA dysregulation in depression, with patients typically showing enhanced ACTH and cortisol responses despite pre-treatment with dexamethasone.
MR/GR Challenge Protocol: To dissect specific receptor contributions, a sequential protocol using receptor-selective compounds can be implemented. Participants receive fludrocortisone (0.4-0.8mg) as an MR agonist, spironolactone (400-800mg) as an MR antagonist, prednisolone (5-10mg) as a mixed MR/GR agonist, and dexamethasone (0.5-1.5mg) as a GR-selective agonist in separate sessions [117]. Plasma cortisol is measured before and 3-24 hours after administration depending on the compound's pharmacokinetics. This protocol can identify specific receptor dysfunction in stress-related disorders.
Psychotherapy Neuroendocrine Assessment Protocol
For trials investigating psychotherapeutic effects on HPA function, a comprehensive assessment includes diurnal cortisol sampling (4-6 timepoints per day over 2 consecutive days), low-dose dexamethasone suppression test (0.25-0.5mg dexamethasone with pre- and post-cortisol measurement), and contextual cortisol assessment during therapy sessions [115]. Salivary cortisol collected immediately before and after therapy sessions can capture acute stress response modulation over the treatment course. For trauma-focused therapies, measuring DHEA(S) alongside cortisol provides additional information about adrenal adaptation, as the cortisol to DHEA ratio may reflect HPA axis balance.
Data Analysis and Interpretation
Statistical Approaches for HPA Data
HPA axis data present unique analytical challenges due to circadian rhythms, pulsatile secretion, and substantial interindividual variability. Mixed-effects models are particularly appropriate for analyzing longitudinal hormone data, accommodating missing timepoints and subject-specific variances. Area under the curve (AUC) analyses should distinguish between AUC with respect to ground (AUCg), reflecting total hormone output, and AUC with respect to increase (AUCi), measuring dynamic change [115]. Piecewise growth curve models can capture biphasic responses to interventions. For pharmacological challenge data, response trajectory analysis using generalized additive models can characterize non-linear response patterns that simple pre-post comparisons might miss.
Interpretation and Clinical Translation
Interpreting HPA-targeted intervention trials requires careful consideration of temporal dissociation between biological and clinical effects. Neuroendocrine changes often precede clinical improvement, suggesting they may represent mechanistically relevant intermediate phenotypes rather than mere correlates of symptom change [115] [113]. Biomarker stratification in analysis can identify subgroups more likely to respond to specific HPA-targeted approaches. For instance, patients with hypercortisolism may show better response to GR antagonists, while those with hypocortisolism might benefit from CRF antagonists or stress response modulation.
The successful development of HPA-targeted interventions requires sophisticated clinical trial methodologies that account for the complexity of neuroendocrine systems. By implementing the designs, endpoints, and analytical approaches outlined in this guide, researchers can more effectively validate the efficacy of novel therapeutics targeting this critical stress response pathway. As our understanding of HPA axis involvement in various disorders continues to evolve, so too will the precision of our clinical trial methodologies, ultimately leading to more targeted and effective treatments for stress-related conditions.
The hypothalamic-pituitary-adrenal (HPA) axis is a primary driver of the neuroendocrine stress response, required for maintaining homeostasis under challenge. Activation of the HPA axis, primarily through neural mechanisms invoking corticotropin-releasing hormone (CRH) from paraventricular nucleus (PVN) neurons, ultimately leads to the secretion of glucocorticoids [1]. These hormones act on multiple organ systems to redirect energy resources to meet real or anticipated demand [1]. The stress response is not monolithic; reactive pathways to direct homeostatic disruption differ from anticipatory pathways driven by upstream limbic structures, with the latter often mediated by trans-synaptic silencing of tonic PVN inhibition [1].
Chronic stress-induced activation of the HPA axis can manifest in various forms—including basal hypersecretion or sensitized stress responses—and is linked to numerous physiological and psychological disease states [1] [118]. Traditionally, stress research has often focused on individual molecular layers. However, the HPA axis orchestrates a system-wide recalibration that cannot be fully understood by studying any single omics layer in isolation. Systems biology, through the integration of multi-omics data, provides a powerful framework to move beyond a reductionist view. By simultaneously analyzing genomics, transcriptomics, proteomics, and metabolomics, researchers can construct a more comprehensive model of the stress response, illuminating the complex interactions between different biological tiers that define an individual's physiological and pathological reaction to stress.
Rationale for Multi-Omics Integration in Stress Research
Stress, defined as a state of threatened homeostasis, elicits a coordinated repertoire of biological, psychological, and behavioral responses [119] [118]. The HPA axis is a key component of this response, but it does not operate in a vacuum. Its activation influences and is influenced by molecular processes across the entire biological spectrum. Figure 1 illustrates the typical workflow for a multi-omics study of the stress response, from data generation to integrated analysis.
Figure 1. Generalized multi-omics workflow for stress research. The process begins with a stress stimulus applied to a model system, followed by multi-omics data acquisition from various biological layers. Computational integration of this data yields systems-level insights into the stress response [120] [121].
Integrating these disparate data types is crucial because each omics layer provides a unique, partial perspective on the system. For example, transcriptomics reveals which genes are being actively transcribed, while proteomics identifies the functional effectors present in the cell, and metabolomics captures the final readout of cellular activity. Crucially, the relationships between these layers are not always linear or predictable; abundant mRNA may not always correlate with high protein levels, and protein abundance may not directly reflect metabolic flux [122]. Multi-omics integration is therefore essential to disentangle these complex, causal relationships and properly capture the emergent phenotype of stress [122].
Computational Integration Strategies
The complexity of multi-omics data presents significant computational challenges. Each omic type has a unique data scale, noise profile, and preprocessing requirements, and the correlations between modalities from the same cell are not yet fully understood [122]. A one-size-fits-all approach does not exist, and the choice of integration strategy must be guided by the experimental design and scientific objective [122] [121].
Types of Data Integration
Integration methods can be broadly categorized based on whether the data is matched or unmatched:
- Matched Integration (Vertical Integration): Data from different omics layers are profiled from the same cell or sample. The sample itself acts as the anchor for integration. This is the ideal scenario and is increasingly common with modern single-cell and spatial technologies [122].
- Unmatched Integration (Diagonal Integration): Data from different omics are drawn from distinct populations of cells or different studies. This requires more sophisticated computational methods to project cells into a shared, co-embedded space to find commonality [122].
- Mosaic Integration: An extension of unmatched integration used when an experimental design has various combinations of omics (e.g., some samples have transcriptomics and proteomics, others have transcriptomics and epigenomics), creating sufficient overlap for integration [122].
Methodologies and Tool Selection
The computational methods for integration are diverse, ranging from statistical models to machine learning approaches. The selection of a specific tool should be dictated by the scientific question. Table 1 summarizes common methodologies and representative tools for key objectives in stress research.
Table 1: Multi-Omics Integration Methods for Key Research Objectives
| Scientific Objective | Description | Common Computational Methods | Example Tools |
|---|---|---|---|
| Subtype Identification | Unsupervised clustering of samples/patients into distinct molecular subtypes, potentially correlating with stress susceptibility or resilience. | Matrix Factorization, Bayesian Models, Neural Networks | MOFA+ [122], LIGER [122] |
| Detect Disease-Associated Molecular Patterns | Identify co-varying features across omics layers that are associated with a stress-related phenotype or pathology. | Similarity Network Fusion, Manifold Alignment, Graph Neural Networks | Spectrum [122], MMD-MA [122] |
| Understand Regulatory Processes | Infer causal or regulatory relationships between molecular layers (e.g., how genetic variation influences chromatin accessibility, which in turn affects gene expression). | Graph-Based Models, Probabilistic Modeling, Variational Autoencoders | CellOracle [122], GLUE [122], SCENIC+ [122] |
These tools address the fundamental challenge of integration: learning a joint representation from separate datasets that can be used for downstream analysis tasks like clustering, classification, and causal inference [121]. For instance, MOFA+ uses a factor analysis model to disentangle the shared and unique sources of variation across multiple omics data sets [122], while GLUE uses a graph-linked unified embedding that incorporates prior biological knowledge to guide the integration of unpaired multi-omics data [122].
Experimental Protocols and Workflows
A representative example of a multi-omics stress study is provided by research on potato plants (Solanum tuberosum, cv. Désirée) subjected to single and combined abiotic stresses (heat, drought, waterlogging) [120]. This study offers a detailed protocol for molecular and physiological profiling.
Detailed Methodology from a Representative Study
1. Stress Application and Phenotyping:
- Stress Regimens: Plants were subjected to heat, drought, and waterlogging as both single stresses and combinations to mimic realistic climate scenarios.
- Deep Phenotyping: Stress responses were monitored via daily, high-throughput physiological measurements. This provided a continuous record of the plant's phenotypic state throughout the stress and recovery periods [120].
2. Multi-Omics Sampling and Data Generation:
- Tissue Sampling: Leaf samples were collected at multiple timepoints during and after the stress treatments.
- Multi-Omics Profiling: The following omics data were generated from the same set of samples:
- Proteomics: To identify and quantify protein abundance.
- Targeted Transcriptomics: To measure gene expression levels.
- Metabolomics: To profile the levels of small-molecule metabolites.
- Hormonomics: To quantify the levels of diverse stress-induced hormones [120].
- Tuber Analysis: Critical metabolites were also analyzed in tuber samples at the end of the stress period to assess impact on the harvestable organ [120].
3. Data Integration and Bioinformatics Analysis:
- Integration Pipeline: A dedicated bioinformatic pipeline was established, based on machine learning and knowledge networks, to integrate the massive, multimodal dataset [120].
- Key Findings: The integrated analysis revealed that waterlogging produced the most dramatic effects, unexpectedly activating ABA (abscisic acid) responses similar to drought. Distinct molecular signatures were identified for heat and drought, and a common downregulation of photosynthesis was observed across all treatments [120].
The logical flow of this experimental design, from stimulus to insight, is captured in Figure 2.
Figure 2. Experimental workflow for a multi-omics stress study. This workflow, as implemented in a plant stress study, highlights the importance of longitudinal design, deep phenotyping, and the application of a specialized computational pipeline for integration [120].
Visualization of Multi-Omics Data and Networks
Effective visualization is critical for interpreting the high-dimensional patterns revealed by multi-omics integration. Networks are a particularly powerful tool for representing complex interactions.
Network Visualization in Psychology and Biology
In psychopathology, networks are used to represent the interconnections between symptoms, where nodes are symptoms and edges are the statistical associations between them [123]. This conceptual framework can be adapted for molecular data, where nodes represent biomolecules (genes, proteins, metabolites) and edges represent regulatory, interaction, or co-variation relationships.
Several algorithms can be used for network visualization, each with advantages and caveats:
- Force-Directed Algorithms (e.g., Fruchterman-Reingold): The most common approach, it creates an aesthetically pleasing layout where connected nodes are pulled together and unconnected nodes are pushed apart. Critically, the spatial arrangement of nodes in such plots is not easily interpretable; distance between nodes does not directly correspond to the strength of their association [123].
- Multidimensional Scaling (MDS): This method represents statistical proximities (e.g., correlations) as distances in a low-dimensional space. In MDS plots, the distance between two nodes is interpretable: highly related nodes appear close together, while weakly related nodes appear far apart [123].
The Scientist's Toolkit: Research Reagent Solutions
Conducting a multi-omics study requires a suite of specialized reagents and platforms for each analytical layer. The following table details key resources for building a multi-omics profiling pipeline.
Table 2: Essential Research Reagents and Platforms for Multi-Omics Stress Research
| Resource Category | Specific Examples / Technologies | Function in Multi-Omics Workflow |
|---|---|---|
| Transcriptomics | RNA-Seq, Single-Cell RNA-Seq, Targeted Transcriptomics | Profiles the complete set of RNA transcripts (coding and non-coding) to measure gene expression dynamics in response to stress [120]. |
| Proteomics | Mass Spectrometry (LC-MS/MS), Antibody Arrays | Identifies and quantifies the full complement of proteins, the key functional effectors in the cell, revealing post-transcriptional regulation [120]. |
| Metabolomics & Hormonomics | Mass Spectrometry (GC-MS, LC-MS), NMR Spectroscopy | Measures the concentrations of small-molecule metabolites and hormones, providing a snapshot of the functional metabolic state and signaling in response to stress [120]. |
| Epigenomics | ATAC-Seq, ChIP-Seq, Bisulfite Sequencing | Maps chromatin accessibility, histone modifications, and DNA methylation, revealing the regulatory landscape that controls gene expression [122]. |
| Public Data Repositories | The Cancer Genome Atlas (TCGA), Answer ALS, jMorp | Provide access to pre-collected, multi-omics datasets from patient samples for validation, comparison, and secondary analysis [121]. |
| Computational Tools | Seurat, MOFA+, GLUE, CellOracle | Software and algorithms for the critical task of integrating, visualizing, and interpreting data from multiple omics layers [122]. |
The integration of multi-omics data represents a paradigm shift in stress research. By moving beyond single-layer analyses, systems biology approaches enable a more holistic and mechanistic understanding of how the HPA axis and associated neuroendocrine systems coordinate a whole-organism response to challenge. The insights gained—into molecular patterns, patient or experimental subtypes, and regulatory networks—are fundamentally inaccessible when omics layers are studied in isolation. As computational methods continue to evolve and multi-omics datasets become more comprehensive and accessible, this integrated approach holds immense promise for identifying novel biomarkers and therapeutic targets for stress-related pathologies, ultimately advancing the goals of precision medicine.
Conclusion
The intricate neuroendocrine interactions centered on the HPA axis represent a critical nexus in stress pathophysiology, with far-reaching implications for understanding and treating a diverse range of conditions from autoimmune diseases to psychiatric disorders. Key insights reveal that HPA axis dysregulation extends beyond simple cortisol imbalances to encompass complex disruptions in feedback mechanisms, receptor sensitivity, and cross-system communications with reproductive, immune, and gut-brain pathways. The developmental programming of the HPA axis underscores the importance of early-life interventions, while sexual dimorphism highlights the need for personalized therapeutic approaches. Future research directions should prioritize longitudinal multi-omics studies to clarify the reversibility of HPA alterations, identify resilience factors, and develop targeted interventions that restore neuroendocrine balance. For drug development professionals, promising avenues include CRH receptor antagonists, glucocorticoid receptor modulators, and microbiota-based therapies that address the systemic nature of stress-related disorders. The integration of HPA axis biomarkers into clinical trial designs will be essential for validating these novel therapeutic strategies and advancing precision medicine in stress-related conditions.
References
- 1. Regulation of the hypothalamic-pituitary-adrenocortical stress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4867107/]
- 2. Physiology of the Hypothalamic–Pituitary–Adrenocortical ... [https://www.sciencedirect.com/science/article/abs/pii/S1567744307002025]
- 3. The Hypothalamic-Pituitary-Adrenal Axis: Development ... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2020.601939/full]
- 4. Paraventricular Hypothalamic Mechanisms of Chronic ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2016.00137/full]
- 5. Heterosynaptic modulation in the paraventricular nucleus ... [https://www.sciencedirect.com/science/article/abs/pii/S0028390818308414]
- 6. Paraventricular nucleus corticotrophin releasing hormone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3118407/]
- 7. Chronic Stress and Autoimmunity: The Role of HPA Axis ... [https://pubmed.ncbi.nlm.nih.gov/41155288/]
- 8. Hypothalamus-pituitary-adrenal and gut-brain axes in ... [https://pubmed.ncbi.nlm.nih.gov/39981404/]
- 9. Pituitary adenylate cyclase-activating peptide [https://en.wikipedia.org/wiki/Pituitary_adenylate_cyclase-activating_peptide]
- 10. Pituitary Adenylate Cyclase-Activating Polypeptide (PACAP ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8395522/]
- 11. Developmental programming and the hypothalamic ... [https://www.sciencedirect.com/science/article/abs/pii/S2451965020300843]
- 12. Developmental origins of the human hypothalamic-pituitary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6334849/]
- 13. Physiology, Stress Reaction - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK541120/]
- 14. Adrenal cortex development and related disorders leading ... [https://www.sciencedirect.com/science/article/pii/S0303720721000502]
- 15. Hypothalamus-pituitary-adrenal and gut-brain axes in ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1541075/full]
- 16. The Interaction of Vasopressin with Hormones of ... - MDPI [https://www.mdpi.com/1422-0067/25/13/7394]
- 17. Central-peripheral neuroimmune dynamics in ... [https://www.nature.com/articles/s41380-025-03085-y]
- 18. Stress responsiveness of the hypothalamic-pituitary ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2013.00026/full]
- 19. Hypothalamic Regulation of Corticotropin-Releasing Factor ... [https://www.mdpi.com/1422-0067/22/22/12242]
- 20. Novel glucocorticoid and cAMP interactions on the CRH ... [https://www.sciencedirect.com/science/article/abs/pii/S0303720702002186]
- 21. Glucocorticoids Inhibit CRH/AVP-Evoked Bursting Activity of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4967125/]
- 22. Stress, hypothalamic-pituitary-adrenal axis ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11535056/]
- 23. Stress and the Reproductive Axis - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4166402/]
- 24. Hypothalamo-pituitary-adrenal axis, sympatho ... [https://pubmed.ncbi.nlm.nih.gov/37724657/]
- 25. The Neuroendocrine Cascade: Where Stress Hijacks ... [https://shopwithmerakico.com/blogs/news/the-neuroendocrine-cascade-where-stress-hijacks-reproductive-signaling]
- 26. Gonads under stress: A systematic review and meta ... [https://www.sciencedirect.com/science/article/pii/S0306453024000489]
- 27. Signalling cognition: the gut microbiota and hypothalamic ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1130689/full]
- 28. Gut Microbiota and the Neuroendocrine System - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5794709/]
- 29. Signalling cognition: the gut microbiota and hypothalamic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10316519/]
- 30. decoding the gut–immune–brain axis in health and disease [https://www.nature.com/articles/s41423-025-01333-3]
- 31. Microbiome Gut-Brain-Axis: Impact on Brain Development and Mental Health | Molecular Neurobiology [https://link.springer.com/article/10.1007/s12035-025-04846-0]
- 32. The gut microbiota, HPA axis, and brain in adolescent-onset ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9758412/]
- 33. The Bidirectional Relationship Between the Gut Microbiome and Mental Health: A Comprehensive Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12007925/]
- 34. Gut microbiome-derived metabolites and epigenetic modulation as potential countermeasures to acute stress | Discover Medicine [https://link.springer.com/article/10.1007/s44337-025-00490-8]
- 35. Gut microbiota regulates stress responsivity via the ... [https://www.sciencedirect.com/science/article/pii/S1550413124003991]
- 36. Gut–Brain Axis and Brain Microbiome Interactions from a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11853140/]
- 37. The Role of Cortisol in Chronic Stress, Neurodegenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10706127/]
- 38. Disrupting Hypothalamic Glucocorticoid Receptors Causes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4061381/]
- 39. Associations between perceived stress and cortisol ... [https://www.nature.com/articles/s41598-025-95603-9]
- 40. Cortisol detection methods for stress monitoring in ... [https://www.sciencedirect.com/science/article/pii/S2772632023000053]
- 41. Dexamethasone/Corticotropin-Releasing Hormone Test [https://emedicine.medscape.com/article/2114213-overview]
- 42. Bioassay Research Methodology: Measuring CRH in Pregnancy [https://pmc.ncbi.nlm.nih.gov/articles/PMC2651683/]
- 43. Normal adrenocorticotropic hormone levels do not exclude ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580128/]
- 44. Hypothalamic-Pituitary-Adrenal (HPA) Axis: What It Is [https://my.clevelandclinic.org/health/body/hypothalamic-pituitary-adrenal-hpa-axis]
- 45. Genetics and epigenetics of stress: New avenues for an old ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9975307/]
- 46. Epigenetic regulation in major depression and other stress ... [https://www.nature.com/articles/s41392-023-01519-z]
- 47. Influence of the HPA Axis on Anxiety-Related Processes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12433346/]
- 48. Preclinical Models of Chronic Stress: Adaptation or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10166771/]
- 49. Translational models of stress and resilience - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12244083/]
- 50. Experimental models of stress - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3181831/]
- 51. The Impact of Chronic Stress on Behavior and Body Mass in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10605805/]
- 52. Editorial: Animal Models of Stress - Current Knowledge ... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2021.655214/full]
- 53. Immune-neuroendocrine crosstalk in mood and psychotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11879693/]
- 54. Glucocorticoid Sensitivity | UCSF SMN [https://www.stressmeasurement.org/glucocorticoid-sensitivity]
- 55. The HPA axis and kynurenine pathway: exploring the role ... [https://link.springer.com/article/10.1007/s43440-025-00806-6]
- 56. Novel molecular insights into the role of CRH type 1 ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295225006951]
- 57. HPA Axis in the Pathomechanism of Depression and ... [https://www.mdpi.com/2076-3425/11/10/1298]
- 58. Progress in Molecular Mechanisms of Depression Induced by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12416060/]
- 59. Reducing stress and alcohol-related behaviors by targeting ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1677510/full]
- 60. Novel selective glucocorticoid receptor modulator GRM-01 ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1542351/full]
- 61. Chronic Stress and Autoimmunity: The Role of HPA Axis ... [https://www.mdpi.com/1422-0067/26/20/9994]
- 62. Stress, hypothalamic-pituitary-adrenal axis ... [https://link.springer.com/article/10.1007/s11011-024-01393-w]
- 63. How to use physical activity to address unhealthy stress [https://lifestylemedicine.org/how-to-use-physical-activity-to-address-unhealthy-stress/]
- 64. Non-pharmacological therapies for chronic stress [https://www.encyclopedie-environnement.org/en/health/non-pharmacological-therapies-for-chronic-stress/]
- 65. Non-Pharmacological interventions for psychological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12273186/]
- 66. Self-care and managing stress and building resilience [https://www.mind.org.uk/information-support/types-of-mental-health-problems/stress/managing-stress-and-building-resilience/]
- 67. Stress & Adrenal Health | Back In Balance [https://backinbalancewnc.com/stress-adrenal-health/]
- 68. An Integrative Approach to HPA Axis Dysfunction [https://pubmed.ncbi.nlm.nih.gov/40499704/]
- 69. Resilience: Build skills to endure hardship [https://www.mayoclinic.org/tests-procedures/resilience-training/in-depth/resilience/art-20046311]
- 70. HPA Axis Dysfunction Symptoms You Shouldn't Ignore [https://www.firststepschiropractic.com/2025/10/26/hpa-axis-dysfunction-symptoms/]
- 71. Best Biomarkers To Test For Hormonal Balance And Energy [https://superpower.com/best-biomarkers/hormonal-balance-energy?srsltid=AfmBOopyud3B2S_rPptQADylLkJWORS-SyqwpxP_NMAZGjogrerjADgh]
- 72. Researchers identify key biomarkers for chronic fatigue ... [https://news.cornell.edu/stories/2025/08/researchers-identify-key-biomarkers-chronic-fatigue-syndrome]
- 73. (PDF) Pharmacological Treatment of Anxiety Disorders: The Role of... [https://www.academia.edu/114692543/Pharmacological_Treatment_of_Anxiety_Disorders_The_Role_of_the_HPA_Axis]
- 74. Frontiers | Gut-brain axis in post-traumatic stress disorder: microbial... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1621678/full]
- 75. Exploring the Molecular Mechanisms of Glucocorticoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4770453/]
- 76. Glucocorticoid Resistance: Interference between the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8465023/]
- 77. Glucocorticoid resistance syndrome: A systematic review of ... [https://www.sciencedirect.com/science/article/abs/pii/S1530891X25012248]
- 78. Glucocorticoid Resistance: Is It a Requisite for Increased ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2019.00423/full]
- 79. Molecular Mechanisms of Glucocorticoid Resistance in ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2020.00021/full]
- 80. Molecular mechanisms contributing to glucocorticoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8992511/]
- 81. Chronic Stress and Autoimmunity: The Role of HPA Axis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563903/]
- 82. An Integrative Approach to HPA Axis Dysfunction [https://www.sciencedirect.com/science/article/pii/S0002934325003535]
- 83. Stress and neuroinflammation: a systematic review of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4828495/]
- 84. Neuroinflammation: The Pathogenic Mechanism of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9147744/]
- 85. Role of neuroinflammation in neurodegeneration ... [https://www.nature.com/articles/s41392-023-01486-5]
- 86. Neuroinflammation and stress-induced pathophysiology in ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2025.1538026/full]
- 87. Early-life experiences and the development of adult diseases with a focus on mental illness: The Human Birth Theory - PubMed [https://pubmed.ncbi.nlm.nih.gov/27235745/]
- 88. Early-Life Stress, HPA Axis Adaptation, and Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4026717/]
- 89. Frontiers | Developmental Trajectories of Early Life Stress and Trauma: A Narrative Review on Neurobiological Aspects Beyond Stress System Dysregulation [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2019.00118/full]
- 90. Broken or maladaptive? Altered trajectories in neuroinflammation and behavior after early life adversity - PubMed [https://pubmed.ncbi.nlm.nih.gov/25081071/]
- 91. Review Prenatal stress and the programming of the HPA axis [https://www.sciencedirect.com/science/article/abs/pii/S0149763409001742]
- 92. Biomarkers of stress resilience: A review [https://www.sciencedirect.com/science/article/pii/S2772408524001170]
- 93. Biomarkers in Stress Related Diseases/Disorders: Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6843074/]
- 94. A bold new approach to autoimmune diseases - JHU Hub [https://hub.jhu.edu/2025/11/17/new-approach-autoimmune-diseases/]
- 95. Dangers of the chronic stress response in the context ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1365871/full]
- 96. Modulation of neuroimmune cytokine networks by ... [https://www.nature.com/articles/s41398-025-03532-y]
- 97. Gut microbiota as a novel target for treating anxiety and ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1664800/full]
- 98. The role of probiotics and prebiotics in modulating of the gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10410452/]
- 99. Why nurturing the gut microbiota could resolve depression ... [https://www.nature.com/articles/d41586-025-02633-4]
- 100. Therapeutic effects and mechanisms of fecal microbiota ... [https://www.sciencedirect.com/science/article/pii/S2405844024092454]
- 101. The interactions between psychological stress, gut microbiota ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12612998/]
- 102. Stress, hypothalamic-pituitary-adrenal axis ... [https://pubmed.ncbi.nlm.nih.gov/39083184/]
- 103. Identification of Neuroendocrine Stress Response-Related ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2018.00132/full]
- 104. Sex differences in the hypothalamic–pituitary–adrenal axis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6235871/]
- 105. Gender difference in hypothalamic–pituitary–adrenal axis ... [https://www.sciencedirect.com/science/article/abs/pii/S0006899397005258]
- 106. Androgens and Their Role in Regulating Sex Differences in ... [https://pubmed.ncbi.nlm.nih.gov/35024695/]
- 107. The microbiota-gut-brain axis in depression - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12507892/]
- 108. The Gut-Brain Axis: Influence of Microbiota on Mood and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6469458/]
- 109. The communication mechanism of the gut-brain axis and ... [https://www.sciencedirect.com/science/article/pii/S0753332224010916]
- 110. neuroimaging as intermediate phenotypes linking genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11755933/]
- 111. Towards precision medicine for stress disorders - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC7192849/]
- 112. Stress across systems and lifespan: emerging biomarkers ... [https://link.springer.com/article/10.1007/s00702-025-03030-x]
- 113. HPA Axis Alterations in Mental Disorders: Impact on Memory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6493879/]
- 114. Efficacy of Treatments Targeting Hypothalamic-Pituitary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8461240/]
- 115. Psychotherapeutic treatment and HPA axis regulation in ... [https://www.sciencedirect.com/science/article/abs/pii/S0306453018303299]
- 116. HPA axis function in alcohol use disorder: A systematic ... [https://www.sciencedirect.com/science/article/pii/S2772392523000573]
- 117. Evaluation of the HPA Axis' Response to Pharmacological ... [https://www.eneuro.org/content/8/1/ENEURO.0222-20.2020]
- 118. Hypothalamic–pituitary–adrenal axis, neuroendocrine ... [https://www.sciencedirect.com/science/article/abs/pii/S0022399902004294]
- 119. Visualization and Semantic Labeling of Mood States Based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9408575/]
- 120. Integration of multi-omics data and deep phenotyping ... [https://pubmed.ncbi.nlm.nih.gov/40173380/]
- 121. A guide to multi-omics data collection and integration for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9747357/]
- 122. A Guide to Multi-omics Integration Strategies [https://frontlinegenomics.com/a-guide-to-multi-omics-integration-strategies/]
- 123. Visualizing Psychological Networks: A Tutorial in R [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2018.01742/full]